Table of Contents
Understanding Placenta Previa Dos and Don’ts
Here is a comprehensive guide on placenta previa dos and don’ts. If you or someone you know is dealing with placenta previa during pregnancy, it’s crucial to understand the necessary precautions and recommendations to ensure a safe and healthy journey. In this article, we will provide you with valuable insights into managing placenta previa effectively.
Definition of Placenta Previa
Placenta previa is a condition where the placenta partially or fully covers the cervix, the opening of the uterus. This can cause bleeding and other complications during pregnancy and delivery, such as premature labor and difficulty delivering the baby. Placenta previa affects about 1 in 200 pregnancies and is more common in women who have had previous cesarean deliveries, multiple pregnancies, or who are carrying twins or triplets.
In a normal pregnancy, the placenta is typically located on the upper or side walls of the uterus. It attaches to the uterine lining and is connected to the developing fetus through the umbilical cord. The placenta plays a vital role in pregnancy by providing oxygen, and nutrients, and removing waste products from the baby’s blood. It also produces hormones that are essential for maintaining pregnancy and supporting fetal growth and development.
Types of placenta previa
Placenta previa is a condition in which the placenta partially or completely covers the cervix, the opening of the uterus. The cervix is the passage through which the fetus is delivered. There are three types of placenta previa:
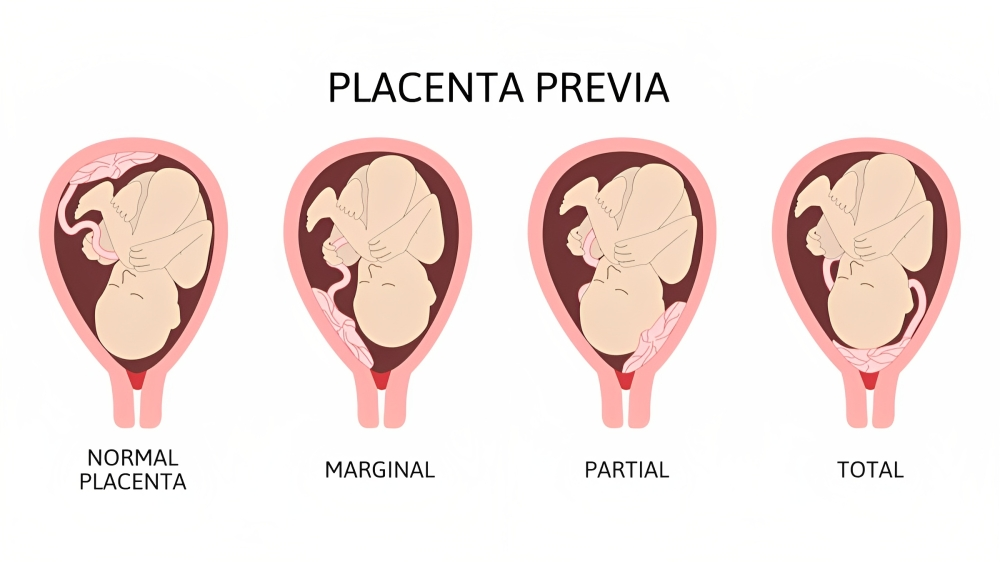
1. Complete placenta previa
- Definition and characteristics: This occurs when the placenta covers the entire cervix. This type of placenta previa is the most severe and usually necessitates a cesarean delivery (c-section).
- Risks and complications associated with complete placenta previa: This type of placenta previa can result in heavy bleeding during pregnancy and delivery. It can also increase the risk of placental abruption, which is the premature separation of the placenta from the uterus before delivery. This can be life-threatening for both the mother and the fetus.
2. Partial placenta previa
- Definition and characteristics: This occurs when the placenta covers part of the cervix. This type of placenta previa may change as the pregnancy advances and the cervix dilates. Sometimes, the placenta may move away from the cervix and allow for a vaginal delivery.
- Risks and complications associated with partial placenta previa: This type of placenta previa can result in bleeding during pregnancy and delivery. It can also increase the risk of preterm labor, infection, and low birth weight for the fetus.
3. Marginal placenta previa
- Definition and characteristics: This occurs when the placenta is near the edge of the cervix but does not cover it. This type of placenta previa is the least severe and usually does not affect delivery.
- Risks and complications associated with marginal placenta previa: This type of placenta previa can result in light bleeding during pregnancy and delivery. It usually does not cause any significant problems for the mother or the fetus.
Causes and risk factors
The exact causes of placenta previa are unknown, but it may be related to how the placenta attaches to the uterus during early pregnancy. Some factors that can increase the likelihood of developing placenta previa are:
- Having had a previous c-section or other surgery on the uterus
- Having had multiple pregnancies or carrying twins or triplets
- Being older than 35 years
- Smoking or using drugs during pregnancy
- Having a history of infertility or using assisted reproductive techniques
Symptoms and complications
The main symptom of placenta previa is vaginal bleeding that can occur at any time during pregnancy, especially in the third trimester. The bleeding can vary from light spotting to heavy bleeding that can soak through pads or clothes. The bleeding can occur without any pain or warning, or it can be triggered by sexual intercourse, vaginal exams, or contractions.
If any vaginal bleeding occurs during pregnancy, it is imperative to contact your doctor immediately or go to the nearest emergency room. Bleeding can be hazardous for you and your fetus and may require prompt treatment.
Some other symptoms or complications that can occur with placenta previa are:
- Pain or discomfort: You may experience some cramping, pressure, or pain in your lower abdomen or back. This can indicate contractions, infection, or placental abruption.
- Complications during labor and delivery: Placenta previa can make labor and delivery more difficult and risky. You may require a c-section to deliver your fetus safely and avoid bleeding. You may also require blood transfusions if you lose a lot of blood. Your fetus may have problems such as prematurity, low birth weight, breathing difficulties, or anemia.
Placenta previa is a serious but manageable condition that can affect your pregnancy and delivery. By following your doctor’s advice and taking precautions, you can reduce the risk of complications and have a safe and healthy pregnancy.
Placenta Previa Dos and Don’ts: How to Have a Safe and Healthy Pregnancy
If you have been diagnosed with placenta previa, you may be feeling anxious and worried about your baby’s health and your own. However, with proper care and management, you can have a safe and healthy pregnancy and delivery. Here are some dos and don’ts to help you cope with placenta previa.
Do get plenty of rest
Placenta previa can cause bleeding at any time during pregnancy, especially in the third trimester. To reduce the risk of bleeding, you should avoid overexertion and strenuous activities, such as exercising, lifting heavy objects, or doing housework. You should also limit your travel and avoid long trips or flights. Rest as much as possible and follow your doctor’s advice on bed rest if needed.
Don’t ignore symptoms
Placenta previa can cause painless vaginal bleeding that can range from light spotting to heavy bleeding. Bleeding can occur spontaneously or after sexual intercourse, vaginal exams, or contractions. Bleeding can also indicate other problems, such as placental abruption or preterm labor.
If you have any vaginal bleeding during pregnancy, you should call your doctor right away or go to the nearest emergency room. Bleeding can be dangerous for you and your baby and may require immediate treatment. You should also watch out for other signs of complications, such as abdominal pain, cramps, contractions, or decreased fetal movements.
Do follow your doctor’s advice on delivery
Placenta previa usually requires a planned cesarean delivery (c-section) before labor starts to prevent bleeding and complications. The optimal timing for a c-section delivery varies depending on different factors, such as the type and location of placenta previa, the amount of bleeding, the gestational age of the baby, and the presence of any other complications. Your doctor will discuss with you the best time and place to deliver your baby.
In some cases, you may need to have a c-section earlier than planned if you have signs of labor, rupture of membranes, bleeding, or fetal distress. You may also need to have steroid injections to help mature your baby’s lungs and prevent respiratory problems after birth.
In rare cases, you may be able to have a vaginal delivery if the placenta previa resolves spontaneously or if the placenta is far enough from the cervical opening. However, this option carries a higher risk of complications and requires careful monitoring and preparation.
Don’t use medicines without asking your doctor
Placenta previa can increase the risk of bleeding and affect how your blood clots. Therefore, you should avoid taking any medicines (including over-the-counter drugs and herbal products) without first asking your doctor. Some medicines can increase bleeding or interfere with blood clottings, such as aspirin, ibuprofen, warfarin, heparin, or ginkgo biloba. You should also avoid smoking or using tobacco products, as they can harm your baby’s health and increase the risk of bleeding.
Do provide physical and emotional support
Placenta previa can be stressful and scary for you and your partner. You may feel anxious about your baby’s well-being and your own. You may also feel isolated or depressed if you have to stay on bed rest for a long time. It is important to seek physical and emotional support from your partner, family, friends, health care providers, or support groups. You can also try relaxation techniques, such as breathing exercises, meditation, or listening to music.
You should also educate yourself about placenta previa and its management. Ask your doctor any questions you have and learn about the possible outcomes and risks. Knowing what to expect can help you cope better and prepare yourself for safe delivery.
Don’t use sex or insert anything into your vagina
Sexual intercourse can trigger bleeding in the placenta previa by irritating the cervix or causing contractions. Therefore, you should avoid sex and any other activities that involve vaginal penetration, such as using tampons, douches, or sex toys. You should also avoid having vaginal exams unless they are necessary for diagnosis or treatment.
Placenta previa is a serious but manageable condition that can affect your pregnancy and delivery. By following these dos and don’ts, you can reduce the risk of complications and improve the outcomes for you and your baby. Remember to consult your doctor if you have any concerns or questions and follow their advice on how to have a safe and healthy pregnancy.
Do Communicate with Healthcare Providers
One of the most important dos for managing placenta previa is to communicate openly and honestly with your healthcare providers. This can help you build a trusting relationship with your healthcare team, share your concerns and questions, and receive the best possible care for you and your baby.
Importance of open and honest communication
Communication is key to having a safe and healthy pregnancy and delivery. By communicating openly and honestly with your healthcare providers, you can:
- Build a trusting relationship with your healthcare team: Your healthcare providers are there to support you and provide you with the best possible care. By communicating openly and honestly with them, you can establish a rapport and trust that can make you feel more comfortable and confident during your pregnancy and delivery.
- Share your concerns and questions: Placenta previa can be stressful and scary, and you may have many concerns and questions about your condition and its management. By communicating openly and honestly with your healthcare providers, you can express your worries and fears, ask any questions you have, and receive accurate and reliable information that can help you cope better.
Sharing all relevant information
Another important do for managing placenta previa is to share all relevant information with your healthcare providers. This can help them diagnose your condition, monitor your progress, and provide you with the most appropriate treatment options.
Some of the information you should share with your healthcare providers are:
- Informing them about your placenta previa condition: If you have been diagnosed with placenta previa by another healthcare provider or facility, you should inform your current healthcare providers about it. This can help them access your medical records, review your ultrasound results, and plan your care accordingly.
- Disclosing any relevant medical history or complications: You should also inform your healthcare providers about any relevant medical history or complications that may affect your pregnancy or delivery. This includes any previous pregnancies or deliveries, any previous surgeries or procedures on the uterus, any chronic conditions or medications you have, or any allergies or reactions you have.
Asking questions and seeking clarification
Another important do for managing placenta previa is to ask questions and seek clarification from your healthcare providers. This can help you understand your condition, its management, and its potential outcomes better.
Some of the questions you may want to ask your healthcare providers are:
- Understanding your treatment options and potential outcomes: You should ask your healthcare providers about the different treatment options available for placenta previa, such as bed rest, medication, blood transfusion, or cesarean delivery. You should also ask them about the potential outcomes of each option, such as the risks and benefits for you and your baby, the success rate, the recovery time, or the long-term effects.
- Clarifying any doubts or uncertainties: You should also ask your healthcare providers to clarify any doubts or uncertainties you may have about placenta previa or its management. For example, you may want to ask them what to expect during labor and delivery, what to do if you have bleeding or other symptoms, how to prepare for cesarean delivery, or how to care for yourself and your baby after delivery.
Seeking a second opinion if needed
Another important do for managing placenta previa is to seek a second opinion if needed. This can help you confirm your diagnosis, explore other treatment options, or feel more confident about your decision.
Some of the situations, when you may want to seek a second opinion, are:
- When to consider seeking a second opinion: You may want to seek a second opinion if you are unsure about your diagnosis, if you are not satisfied with the treatment options offered by your current healthcare provider, if you have conflicting opinions from different healthcare providers, or if you want to explore other alternatives.
- Steps to take when seeking a second opinion: You should inform your current healthcare provider that you want to seek a second opinion and ask them for a referral or recommendation. You should also request copies of your medical records and ultrasound results. You should then contact the second healthcare provider and schedule an appointment. You should prepare a list of questions to ask them and compare their opinions with those of your current healthcare provider.
Preparing for Labor and Delivery
Another important aspect of managing placenta previa is to prepare for labor and delivery. This can help you reduce the risk of complications and improve the outcomes for you and your baby.
Creating a birth plan
One of the ways to prepare for labor and delivery is to create a birth plan. A birth plan is a document that outlines your preferences and expectations for labor and delivery. It can help you communicate with your healthcare team and make informed decisions.
Some of the things you may want to include in your birth plan are:
- Discussing delivery preferences with your healthcare team: You should discuss your delivery preferences with your healthcare team and make sure they are aware of your placenta previa condition. You should also ask them about their policies and procedures for managing placenta previa and how they will handle any emergencies or complications.
- Considering potential scenarios and interventions: You should also consider the potential scenarios and interventions that may occur during labor and delivery and how you feel about them. For example, you may want to think about whether you want to have a vaginal delivery or a cesarean delivery, whether you want to have pain relief or not, whether you want to have a blood transfusion or not, or whether you want to have skin-to-skin contact or delayed cord clamping with your baby.
Discussing delivery options with healthcare providers
Another way to prepare for labor and delivery is to discuss your delivery options with your healthcare providers. This can help you understand the pros and cons of each option and make the best choice for you and your baby.
Some of the delivery options you may want to discuss with your healthcare providers are:
- Vaginal delivery vs. cesarean section: Weighing the options: Placenta previa usually requires a cesarean section to deliver the baby safely and avoid bleeding. However, in some cases, vaginal delivery may be possible if the placenta is far enough from the cervix or if it moves away from the cervix as the pregnancy progresses. You should discuss with your healthcare providers the advantages and disadvantages of each option, such as the recovery time, the risk of infection, the impact on future pregnancies, or the bonding experience with your baby.
- Understanding the risks and benefits of each delivery method: You should also understand the risks and benefits of each delivery method for you and your baby. For example, a cesarean section can reduce the risk of bleeding and fetal distress, but it can also increase the risk of infection, blood clots, or injury to other organs. A vaginal delivery can reduce the risk of infection, blood clots, or injury to other organs, but it can also increase the risk of bleeding, fetal distress, or uterine rupture.
Knowing when to seek medical assistance during labor
Another way to prepare for labor and delivery is to know when to seek medical assistance during labor. This can help you prevent or manage any complications that may arise during labor.
Some of the situations, when you should seek medical assistance during labor, are:
- Recognizing signs of complications during labor: You should seek medical assistance during labor if you notice any signs of complications, such as heavy bleeding, severe pain, fever, chills, foul-smelling discharge, or decreased fetal movements.
- Understanding emergency protocols and when to call for help: You should also understand the emergency protocols and when to call for help during labor. For example, you should know how to contact your healthcare provider or emergency services, how to monitor your vital signs and fetal heart rate, how to stop or slow down bleeding, or how to perform CPR on your baby if needed.
Understanding potential complications and interventions
Another way to prepare for labor and delivery is to understand the potential complications and interventions that may occur during labor and delivery. This can help you anticipate any challenges and be prepared for any medical interventions or treatments.
Some of the potential complications and interventions that may occur during labor and delivery are:
- Anticipating potential challenges and complications: You should anticipate some of the potential challenges and complications that may occur during labor and delivery, such as preterm labor, placental abruption, fetal distress, postpartum hemorrhage, or infection.
- Knowing the available medical interventions and treatments: You should also know the available medical interventions and treatments that may be used to manage these complications, such as medication, blood transfusion, cesarean section, hysterectomy, or neonatal intensive care unit (NICU).
Emotional Support and Coping Strategies
Another important aspect of managing placenta previa is to seek emotional support and coping strategies. Placenta previa can be emotionally stressful and challenging for you and your partner. You may feel anxious, scared, depressed, isolated, or guilty. It is important to seek emotional support and coping strategies to help you deal with these feelings and improve your well-being.
Dealing with anxiety and stress
One of the ways to seek emotional support and coping strategies is to deal with anxiety and stress. Anxiety and stress can affect your physical and mental health and interfere with your pregnancy and delivery.
Some of the ways to deal with anxiety and stress are:
- Recognizing the emotional impact of placenta previa: You should recognize that placenta previa can have a significant emotional impact on you and that it is normal to feel anxious or stressed about it. You should not blame yourself or feel guilty for having placenta previa. You should also acknowledge your feelings and emotions and express them in healthy ways.
- Coping mechanisms to reduce stress and anxiety: You should also use coping mechanisms to reduce stress and anxiety, such as breathing exercises, meditation, yoga, massage, aromatherapy, music, reading, or hobbies. You should also avoid triggers that can increase your stress and anxiety, such as negative news, social media, or toxic people. You should also practice positive affirmations, gratitude, and optimism to boost your mood and confidence.
Building a support network
Another way to seek emotional support and coping strategies is to build a support network. A support network is a group of people who can provide you with emotional, practical, or informational support during your pregnancy and delivery.
Some of the ways to build a support network are:
- Seeking support from family, friends, or support groups: You should seek support from your family, friends, or support groups who can listen to you, comfort you, encourage you, or help you with your daily needs. You should also communicate your needs and expectations to them and let them know how they can best support you.
- Engaging with professionals specializing in emotional support: You should also engage with professionals who specialize in emotional support, such as counselors, therapists, social workers, or psychologists. They can help you cope with your emotions, provide you with guidance and advice, or refer you to other resources or services.
Connecting with other women who have experienced placenta previa
Another way to seek emotional support and coping strategies is to connect with other women who have experienced placenta previa. Connecting with other women who have experienced placenta previa can help you feel less alone, share your experiences and feelings, learn from their stories and insights, or find hope and inspiration.
Some of the ways to connect with other women who have experienced placenta previa are:
- Online communities and forums for sharing experiences: You can join online communities and forums where you can share your experiences and feelings with other women who have experienced placenta previa. You can also read their posts and comments and learn from their experiences and tips. Some of the online communities and forums for placenta previa are the Placenta Previa Support Group on Facebook, Placenta Previa Forum on BabyCenter, and Placenta Previa Community on What to Expect.
- Peer support groups and local organizations: You can also join peer support groups or local organizations where you can meet other women who have experienced placenta previa in person or virtually. You can also participate in their activities and events and benefit from their support and resources. Some of the peer support groups or local organizations for placenta previa are Placenta Previa Foundation, Placenta Previa Association, and Placenta Previa Support Network.
Postpartum Care and Recovery
Another important aspect of managing placenta previa is to take care of yourself and your baby after delivery. Postpartum care and recovery can help you heal physically and emotionally and prevent any complications or infections.
Monitoring for postpartum bleeding
One of the ways to take care of yourself after delivery is to monitor for postpartum bleeding. Postpartum bleeding is normal after delivery and usually lasts for a few weeks. However, excessive bleeding can be a sign of a problem and may require medical attention.
Some of the things you should do to monitor for postpartum bleeding are:
- Understanding normal postpartum bleeding vs. excessive bleeding: You should understand what is normal postpartum bleeding vs. excessive bleeding. Normal postpartum bleeding is usually bright red at first and then gradually changes to brown or yellow. It may also contain clots or tissue. Excessive bleeding is when you soak through more than one pad per hour, pass large clots or tissue, have foul-smelling discharge, or feel dizzy or weak.
- When to seek medical attention during the postpartum period: You should seek medical attention during the postpartum period if you have excessive bleeding or any signs of infection, such as fever, chills, pain, swelling, or redness. You should also seek medical attention if you have any signs of postpartum depression or anxiety, such as sadness, hopelessness, guilt, anger, irritability, loss of interest, insomnia, appetite changes, or thoughts of harming yourself or your baby.
Rest and recovery recommendations
Another way to take care of yourself after delivery is to rest and recover. Rest and recovery can help you heal faster and regain your strength and energy.
Some of the tips for postpartum rest and recovery are:
- Importance of rest for healing and recovery: You should rest as much as possible after delivery and avoid any strenuous activities or heavy lifting. You should also limit your visitors and ask for help from your partner, family, friends, or caregivers. Resting can help your body heal faster and prevent any complications or infections.
- Tips for postpartum self-care and well-being: You should also take care of yourself physically and emotionally after delivery. You should eat a balanced diet rich in iron, protein, calcium,
References
(1) Placenta Previa Dos & Don’ts, Symptoms, & What To Expect At Birth.
(2) Placenta previa – Symptoms and causes – Mayo Clinic.
(3) Placenta Previa | Diagnosis & Treatment | Denver & Colorado – UCHealth.
(4) Placenta Previa – Carle.org.