A nursing care plan for a C-section delivery is a crucial part of ensuring a safe and healthy recovery for both the mother and the baby. C-sections are surgical procedures that require specific care and attention to prevent complications and promote healing. A nursing care plan typically includes interventions and strategies for managing pain, promoting mobility, preventing infection, and providing emotional support during the postpartum period.
Table of Contents
What is C-Section?
A C-section, short for Cesarean section, is a surgical procedure in which a baby is delivered through an incision made in the mother’s abdomen and uterus. This procedure is typically done when a vaginal delivery poses a risk to the mother or the baby, or when a vaginal delivery is not possible.
Most Common Reasons for C-Section
There are several reasons why a C-section, may be recommended over a vaginal delivery. Here are some of the most common reasons:
- Previous C-section: Women who have had a previous C-section may be advised to have a repeat C-section, as attempting a vaginal delivery can pose risks to both the mother and the baby.
- Labor complications: If labor is not progressing as it should or there are complications such as a breech presentation, a C-section may be necessary.
- Fetal distress: If the baby is showing signs of distress, such as a slowed heart rate or lack of oxygen, a C-section may be performed to ensure safe delivery.
- Multiple pregnancies: Women carrying twins, triplets, or more may require a C-section if there are concerns about the position or health of the babies.
- Maternal health conditions: Certain maternal health conditions, such as high blood pressure or diabetes, may make a vaginal delivery risky and a C-section a safer option.
- Placenta problems: If the placenta is covering the cervix or separating from the uterus, a C-section may be necessary to prevent complications such as hemorrhaging.
- Large baby: If the baby is estimated to be larger than average, a C-section may be recommended to avoid shoulder dystocia or other complications during delivery.
Types of C-Section
The different types of C-sections include:
- Emergency C-section: This is performed when there is a sudden, unexpected complication that requires immediate delivery of the baby. Examples of emergency situations may include fetal distress, placental abruption, or uterine rupture.
- Planned C-section: This is scheduled in advance and may be recommended for various reasons, such as previous C-sections, multiple pregnancies, certain medical conditions, or fetal abnormalities.
- Repeat C-section: This is performed when a woman has had a previous C-section delivery and is recommended to have another C-section for a subsequent pregnancy.
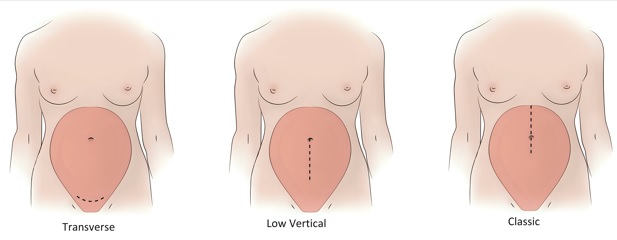
- Classical C-section: This involves a vertical incision made in the uterus and is rarely performed due to higher risks of complications, such as bleeding and future uterine rupture.
- Low-transverse C-section: This is the most common type of C-section performed. It involves a horizontal incision made in the lower part of the uterus, which is less likely to cause complications and allows for future vaginal births after a C-section (VBAC).
- T-shaped C-section: This involves a horizontal incision across the lower uterus, as well as a vertical incision extending down the uterus, and is typically performed in cases of abnormal fetal positioning or certain medical conditions.
Nursing Care Plan For C-Section
It is important to have a nursing care plan in place to ensure that the mother and baby receive appropriate care before, during, and after the surgery. Here, we will discuss the nursing care plan for C-sections, including assessments, interventions, and evaluations.
- Preoperative Assessment
Before a C-section, the nurse will assess the mother’s health status and document her medical history. The nurse will also perform a physical examination, including vital signs, abdominal assessment, and fetal monitoring. The nurse should assess the mother’s emotional state, provide education about the procedure, and answer any questions the mother may have. - Preoperative Interventions
The nurse should administer medications as ordered, such as antibiotics, antacids, and antiemetics. The nurse should also ensure that the mother has an empty stomach by restricting oral intake for several hours before the procedure. The nurse should confirm that informed consent has been obtained and that the surgical site has been marked appropriately. - Intraoperative Care
During the C-section, the nurse will provide emotional support to the mother and monitor vital signs. The nurse will ensure that the surgical team has all necessary supplies and equipment, including blood products if needed. The nurse will document the procedure and monitor the mother for any complications. - Postoperative Assessment
After the C-section, the nurse will assess the mother’s vital signs, pain level, and incision site. The nurse will monitor the mother for complications such as bleeding, infection, and thrombophlebitis. The nurse will also assess the baby’s vital signs, weight, and feeding status. - Postoperative Interventions
The nurse will provide pain management, wound care, and assistance with breastfeeding. The nurse will encourage the mother to ambulate and perform deep breathing exercises to prevent complications. The nurse will provide education about postoperative care and follow-up appointments. - Evaluation
The nurse will evaluate the effectiveness of the nursing care plan by assessing the mother and baby’s progress, monitoring for complications, and documenting outcomes. The nurse will revise the nursing care plan as necessary based on the evaluation. - Pain Management
Pain management is an essential component of nursing care for C-section patients. The nurse should assess the mother’s pain level frequently and administer medications as ordered. The nurse should also use non-pharmacological interventions such as relaxation techniques and positioning to help manage pain. - Wound Care
The nurse should assess the incision site frequently for signs of infection or dehiscence. The nurse should provide wound care as ordered, such as dressing changes and irrigation. The nurse should also monitor for signs of thrombophlebitis and implement interventions to prevent deep vein thrombosis. - Breastfeeding Support
The nurse should provide education about breastfeeding and assist the mother with latching and positioning. The nurse should assess the baby’s feeding status and provide appropriate interventions if necessary. The nurse should also monitor the mother for signs of breast engorgement or mastitis. - Emotional Support
The nurse should provide emotional support to the mother and family before, during, and after the C-section. The nurse should assess the mother’s emotional state and provide appropriate interventions, such as referrals to social services or counseling. - Prevention of Complications
The nurse should implement interventions to prevent complications such as infection, bleeding, and thromb - Ambulation and Exercise
The nurse should encourage the mother to ambulate as soon as possible after the C-section to prevent complications such as pneumonia, thrombophlebitis, and atelectasis. The nurse should also provide education about safe exercise and activity levels during the postoperative period. - Nutrition and Hydration
The nurse should monitor the mother’s intake and output and assess for signs of dehydration or electrolyte imbalance. The nurse should provide education about appropriate nutrition and hydration during the postoperative period. - Medication Management
The nurse should ensure that the mother receives medications as ordered, including pain management, prophylaxis for deep vein thrombosis, and antibiotics as necessary. The nurse should monitor for medication interactions and adverse effects and document administration and effectiveness. - Follow-up Care
The nurse should provide education about follow-up care, including appointments with healthcare providers, warning signs of complications, and postoperative care of the incision site. The nurse should also provide information about contraception and family planning.
Nursing Diagnosis for C-Section
- Disturbed Body Image r/t surgery, unmet expectations for childbirth
- Interrupted Family processes r/t unmet expectations for childbirth
- Fear r/t perceived threat to own well-being, the outcome of birth
- Impaired physical Mobility r/t pain
- Acute Pain r/t surgical incision
- Ineffective Role performance r/t unmet expectations for childbirth
- Situational low Self-Esteem r/t inability to deliver child vaginally
- Risk for Bleeding: Risk factor: surgery
- Risk for imbalanced Fluid volume: Risk factors: loss of blood, fluid shifts
- Risk for Infection: Risk factor: surgical incision
- Risk for Urinary Retention: Risk factor: regional anesthesia
- Readiness for enhanced Childbearing process: a pattern of preparing for, maintaining, and strengthening care of newborn
- Readiness for enhanced Knowledge: expresses an interest in learning
Acute Pain r/t surgical incision
Assessment:
In this case, the patient is experiencing acute pain related to a surgical incision from a Cesarean section (C-section). The patient reports pain at the incision site that is sharp and stabbing in nature, with a pain rating of 8 out of 10.
Evidenced by:
- The patient reports pain at the incision site
- Pain is described as sharp and stabbing
- The pain rating is 8 out of 10
- The patient has limited movement due to pain
- The patient is anxious and restless due to pain.
Expected Outcome:
The expected outcome for the nursing diagnosis of Acute Pain is for the patient to experience a reduction in pain intensity and improved comfort levels. The patient will be able to move more freely without pain and will be able to participate in activities of daily living without discomfort.
Acute Pain – Nursing Interventions and Rationale:
- Administer pain medication as prescribed by the healthcare provider. This will help to reduce pain intensity and improve comfort levels, allowing the patient to move more freely and participate in activities of daily living without discomfort.
- Encourage the patient to use relaxation techniques, such as deep breathing and progressive muscle relaxation. This will help to reduce anxiety and tension, which can exacerbate pain levels.
- Position the patient in a comfortable position that promotes healing and reduces pressure on the incision site. This may involve using pillows to support the patient’s back or elevating their legs to reduce swelling.
- Educate the patient about the importance of wound care and hygiene, including how to properly clean and dress the incision site. This will help to prevent infection and promote healing.
- Encourage the patient to engage in distractions, such as reading, listening to music, or watching TV, to take their mind off the pain. This can help to reduce pain intensity and improve comfort levels.
Evaluation:
The effectiveness of nursing interventions should be evaluated regularly to determine if the expected outcome is being achieved. This can be done by assessing the patient’s pain levels and comfort levels, as well as their ability to move and participate in activities of daily living without discomfort.
If the patient reports a reduction in pain intensity, improved comfort levels, and increased ability to move and participate in activities of daily living without discomfort, then the nursing interventions have been successful. If the patient continues to experience high levels of pain or discomfort, then the nursing interventions should be re-evaluated and revised as needed.
Impaired physical Mobility r/t pain
Assessment:
Impaired Physical Mobility is a nursing diagnosis that refers to the inability to move freely and independently. In this case, the patient is experiencing impaired physical mobility related to pain following a Cesarean section (C-section). The patient reports pain at the incision site that is limiting their ability to move, walk and perform activities of daily living.
Evidenced by:
The patient reports pain at the incision site
Pain is described as severe and sharp in nature
The patient reports difficulty moving, walking, and performing activities of daily living due to pain
The patient is using a wheelchair or assistive device for mobility
The patient reports feeling anxious and depressed due to their limited mobility.
Expected Outcome:
The expected outcome of the nursing diagnosis of Impaired Physical Mobility is for the patient to experience improved mobility and independence. The patient will be able to walk and perform activities of daily living without significant pain or assistance.
Impaired Mobility – Nursing Interventions and Rationale:
1. Administer pain medication as prescribed by the healthcare provider. This will help to reduce pain levels and improve the patient’s ability to move and participate in activities of daily living.
2. Encourage the patient to use a pillow or abdominal binder to support the incision site while moving or walking, which can reduce pain levels and improve mobility.
3. Assess the patient’s environment for safety hazards and make modifications as needed to reduce the risk of falls and injuries. This may involve installing grab bars, ramps, or other assistive devices to help the patient move safely and independently.
4. Educate the patient and family members about proper body mechanics and techniques for lifting and transferring, which can reduce the risk of injury and pain.
5. Encourage the patient to engage in regular physical therapy and exercise programs to improve strength and flexibility, which can reduce pain levels and improve mobility.
Evaluation:
The effectiveness of nursing interventions should be evaluated regularly to determine if the expected outcome is being achieved. This can be done by assessing the patient’s ability to move and participate in activities of daily living without significant pain or assistance, as well as their use of assistive devices.
If the patient reports improved mobility and independence, reduced pain levels, and appropriate use of assistive devices, then the nursing interventions have been successful. If the patient continues to experience impaired physical mobility or high levels of pain, then the nursing interventions should be re-evaluated and revised as needed.
Fear r/t perceived threat to own well-being, the outcome of birth
Assessment:
Fear is a nursing diagnosis that refers to an emotional response to perceived or actual danger. In this case, the patient is experiencing fear related to their C-section and the outcome of their birth. The patient reports feeling anxious and fearful about the procedure, as well as concerned about their own well-being and the well-being of their baby.
Evidenced by:
- The patient reports feeling anxious and fearful about the C-section procedure
- Patient expresses concerns about their own well-being and the well-being of their baby
- The patient is tearful and appears agitated
- The patient’s vital signs are elevated, including heart rate and blood pressure
- The patient has difficulty sleeping and eating due to anxiety.
Expected Outcome:
The expected outcome for the nursing diagnosis of Fear is for the patient to experience a reduction in anxiety and fear related to the C-section and the outcome of their birth. The patient will be able to verbalize their concerns and fears, as well as identify coping strategies to manage their anxiety.
Fear – Nursing Interventions and Rationale:
- Provide emotional support and reassurance to the patient, as well as information about the C-section procedure and what to expect. This can help to alleviate anxiety and fears related to the unknown.
- Encourage the patient to verbalize their concerns and fears, and provide a safe space for them to express their emotions. This can help the patient feel heard and validated.
- Teach the patient relaxation techniques such as deep breathing, guided imagery, and progressive muscle relaxation. These techniques can help to reduce anxiety and promote relaxation.
- Involve the patient’s partner or support person in the care and education process. This can help the patient feel supported and reduce feelings of isolation.
- Collaborate with the healthcare team to develop a plan of care that addresses the patient’s fears and concerns, and provides opportunities for the patient to participate in decision-making about their care.
Evaluation:
The effectiveness of nursing interventions should be evaluated regularly to determine if the expected outcome is being achieved. This can be done by assessing the patient’s anxiety levels, vital signs, and ability to verbalize their concerns and fears. If the patient reports a reduction in anxiety and fear, as well as the ability to identify coping strategies to manage their anxiety, then the nursing interventions have been successful. If the patient continues to experience high levels of anxiety and fear, then the nursing interventions should be re-evaluated and revised as needed.
Disturbed Body Image r/t surgery, unmet expectations for childbirth
Assessment:
Disturbed Body Image is a nursing diagnosis that refers to an individual’s negative perception of their physical appearance, which can lead to emotional distress, decreased self-esteem, and social isolation.
In this case, the patient is experiencing a disturbed body image following surgery and unmet expectations for childbirth. The patient expresses dissatisfaction with her physical appearance due to scarring from surgery and changes to her body following childbirth.
Evidenced by:
- Patient expresses dissatisfaction with physical appearance and negative feelings towards their body
- The patient avoids looking in the mirror or engaging in activities that involve physical appearance
- Patient reports feeling embarrassed or self-conscious in public due to their physical appearance
- The patient is experiencing anxiety and depression related to their negative body image
- The patient is experiencing difficulty with sexual relationships due to their negative body image.
Expected Outcome:
The expected outcome for the nursing diagnosis of Disturbed Body Image is for the patient to develop a more positive perception of their physical appearance and improved self-esteem. The patient will feel comfortable engaging in social activities that involve their physical appearance and will have improved sexual relationships.
Disturbed Body Image – Nursing Interventions and Rationale:
- Develop a therapeutic relationship with the patient to create a supportive environment where they can express their concerns and fears without judgment. This will help to build trust and rapport with the patient and will provide an opportunity for the nurse to understand the patient’s perspective and feelings.
- Encourage the patient to verbalize their feelings and concerns related to their negative body image. This will help the patient to identify the root cause of their negative body image and develop strategies to address it.
- Provide education to the patient about the normal physical changes that occur after surgery and childbirth. This will help to reduce anxiety and provide the patient with realistic expectations about their physical appearance.
- Collaborate with the healthcare team to develop a plan for scar management and/or other interventions to improve the patient’s physical appearance. This will help the patient to feel more in control of their body and improve their self-esteem.
- Encourage the patient to engage in activities that promote positive body images, such as exercise or self-care. This will help the patient to feel more confident and positive about their physical appearance.
Evaluation:
This can be done by assessing the patient’s verbalization of their feelings related to their body image, as well as observing their behavior related to social activities and sexual relationships.
If the patient reports feeling more positive about their physical appearance, engaging in social activities, and having improved sexual relationships, then the nursing interventions have been successful. If the patient continues to express negative feelings about their body image, then the nursing interventions should be re-evaluated and revised as needed
You May Also Like
Nursing Care Plan for Acute Pain
Nursing Care Plan for Postpartum Hemorrhage
Nursing Care Plan for Hypertension