Table of Contents
Beck’s Triad and the Significance in Cardiac Health
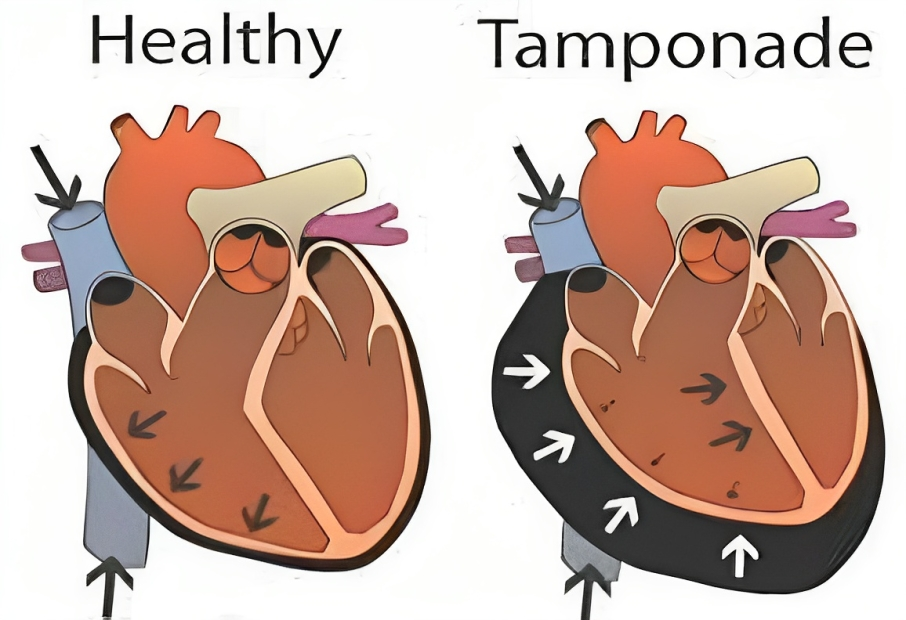
Beck’s triad is a set of three clinical signs that can be indicative of a life-threatening condition known as cardiac tamponade. This serious condition occurs when there is an excessive accumulation of fluid, blood, or air within the pericardium, the sac that surrounds the heart. As a result, the heart experiences increased pressure, hindering its ability to effectively pump blood. Cardiac tamponade can have various underlying causes, including chest trauma, infection, heart attack, or kidney failure.
The three hallmark signs of Beck’s triad are:
- Low Blood Pressure: When the heart struggles to pump an adequate amount of blood to the body, it results in low blood pressure. This can lead to symptoms like dizziness, fainting, weakness, and anxiety.
- Distended Neck Veins: The accumulation of fluid in the pericardium obstructs the return of blood from the veins to the heart. This obstruction causes the veins in the neck to become swollen and visibly pronounced, a sign that can be detected through physical examination.
- Muffled Heart Sounds: The presence of fluid in the pericardium dampens the audibility of heartbeats, making them challenging to hear with a stethoscope.

Beck’s triad was first described by Claude Beck, a prominent American cardiothoracic surgeon, in 1935. It’s important to note, however, that not all cases of cardiac tamponade manifest with Beck’s triad. Only a minority of patients exhibit all three signs upon diagnosis. Therefore, while Beck’s triad can be a valuable clinical clue, it’s not a foolproof diagnostic tool for cardiac tamponade; rather, it serves as an alert to clinicians to consider this possibility.
Diagnosis and Treatment of Cardiac Tamponade
Cardiac tamponade is a medical emergency that demands immediate attention. Left untreated, it can lead to shock, organ failure, and even death. The diagnosis of cardiac tamponade hinges on clinical suspicion, a thorough medical history, physical examination, and imaging tests. The most commonly employed imaging technique to confirm cardiac tamponade is an echocardiogram. This non-invasive test employs sound waves to create a visual representation of the heart and its structures. An echocardiogram can effectively reveal the volume and location of the fluid within the pericardium and assess its impact on heart function.
The treatment of cardiac tamponade is contingent on its cause and severity. The primary objective of treatment is to alleviate the pressure on the heart and reinstate normal blood flow. This is typically accomplished by extracting the excess fluid from the pericardium through a procedure known as pericardiocentesis. This procedure entails the insertion of a needle into the chest to drain the fluid. In certain cases, surgery may be required to create an opening in the pericardium or remove a portion of it to prevent further fluid accumulation.
Complications and Prognosis of Cardiac Tamponade
Cardiac tamponade can lead to grave complications if not treated promptly. These complications may encompass:
- Cardiogenic Shock: This condition arises when the heart is unable to pump sufficient blood to meet the body’s requirements, resulting in low blood pressure and damage to vital organs.
- Pulmonary Edema: Fluid may back up into the lungs, causing breathing difficulties and reduced oxygen levels.
- Arrhythmias: Abnormal heart rhythms can affect heart rate and blood flow.
- Cardiac Arrest: This occurs when the heart ceases to beat entirely.
The prognosis of cardiac tamponade is subject to multiple factors, including the underlying cause, the quantity of fluid in the pericardium, and the timeliness of diagnosis and treatment. The mortality rate associated with cardiac tamponade varies widely, spanning from 10% to 85%, contingent on these variables. Early recognition and intervention are pivotal in enhancing survival rates and overall patient outcomes.
Beck’s Triad Vs Cushing’s Triad
| Aspect | Beck’s Triad | Cushing’s Triad |
|---|---|---|
| Associated Condition | Cardiac Tamponade | Increased Intracranial Pressure (ICP) |
| Components | 1. Low Blood Pressure 2. Distended Neck Veins 3. Muffled Heart Sounds | 1. Hypertension 2. Bradycardia (slow heart rate) & widening of pulse pressure 3. Irregular Respirations |
| Clinical Significance | Indicative of cardiac tamponade, a life-threatening cardiac emergency. | Indicative of severe brain ischemia and potential imminent brain herniation |
| Causes | Cardiac tamponade due to fluid or blood accumulation in the pericardium. | Elevated intracranial pressure due to conditions such as head injury, tumor, infection, or hemorrhage. |
| Cardiac Assessment | Focuses on cardiac parameters such as blood pressure, heart sounds, and neck vein distension. | Focuses on neurological parameters, including heart rate, respiratory pattern, and neurological status. |
| Primary Care Setting | Often seen in cardiac or critical care units, as it’s related to cardiac issues. | Typically seen in neurocritical care units or emergency departments. |
| Diagnostic Tools | Echocardiogram for confirmation, chest X-rays, and physical examination. | Clinical evaluation, head CT or MRI, and intracranial pressure monitoring. |
| Intervention | Emergency pericardiocentesis to remove excess fluid from the pericardium. | Treat the underlying cause of increased ICP, such as head trauma or tumors. |
| Prognosis | Prompt treatment is crucial to prevent further cardiac complications. | Early recognition and intervention are essential to prevent brain damage. |
Nurse’s Responsibilities in Beck’s Triad and Cardiac Tamponade
Nurses play a crucial role in the assessment, monitoring, and care of patients with Beck’s Triad and cardiac tamponade. These responsibilities include:
- Assessment and Monitoring:
- Regular monitoring of vital signs, including blood pressure, heart rate, and respiratory rate, to detect signs of Beck’s Triad and cardiac tamponade.
- Frequent neurological assessments to gauge changes in consciousness, level of alertness, and pupil reactivity.
- Continuous assessment of respiratory status, including the presence of dyspnea, labored breathing, and chest discomfort.
- Cardiovascular Monitoring:
- Frequent monitoring of the patient’s heart rate and rhythm, using ECG or telemetry, to detect any arrhythmias or changes in cardiac status.
- Assessing for distended neck veins is a key clinical sign of Beck’s Triad.
- Pulmonary Assessment:
- Monitoring for signs of respiratory distress, such as tachypnea, use of accessory muscles, and the presence of crackles on auscultation.
- Assessment of oxygen saturation (SpO2) to ensure adequate oxygenation.
- Fluid Balance Management:
- Monitoring input and output (I/O) to maintain fluid balance and prevent overhydration.
- Ensuring proper administration of intravenous fluids and medications, as prescribed.
- Pain Management:
- Assessing and managing the patient’s pain and discomfort, as cardiac tamponade can cause chest pain and anxiety.
- Patient Education:
- Educating the patient and their family about the condition, the need for prompt reporting of symptoms, and the importance of adhering to the treatment plan.
- Emergency Response:
- Being prepared to initiate life-saving interventions if the patient’s condition deteriorates rapidly, such as calling a “code blue” or “rapid response.”
- Assisting with Procedures:
- Assisting with pericardiocentesis, a procedure to remove excess fluid from the pericardium.
- Monitoring the patient during and after pericardiocentesis for any adverse reactions.
- Documentation:
- Maintaining accurate and detailed records of assessments, interventions, and the patient’s response to treatment. Comprehensive documentation is essential for tracking changes and ensuring continuity of care.
- Collaboration:
- Collaborating closely with the healthcare team, including cardiologists, interventional radiologists, and surgeons, to ensure coordinated care and interventions.
- Support and Communication:
- Providing emotional support to the patient and their family, as coping with a life-threatening cardiac condition can be distressing.
- Follow-Up Care:
- Ensuring appropriate follow-up care and outpatient management post-procedure or hospitalization.
Nurses play a pivotal role in the early recognition, management, and ongoing care of patients with Beck’s Triad and cardiac tamponade. Their vigilance, assessment skills, and prompt interventions can significantly impact patient outcomes and contribute to a better quality of life for those affected by these conditions.
In Conclusion
Beck’s triad serves as a vital clinical sign that may indicate the presence of cardiac tamponade, a grave condition characterized by an excess of fluid within the pericardial sac surrounding the heart. While Beck’s triad is a valuable alert, it is not universally present and does not serve as a definitive diagnostic tool for cardiac tamponade. Confirmation of the diagnosis often requires additional tests, particularly echocardiography. The timely and appropriate treatment of cardiac tamponade is essential, involving the removal of excess fluid from the pericardium to alleviate pressure on the heart and restore normal blood flow. Failure to address cardiac tamponade promptly can lead to severe complications and a heightened risk of mortality.