Table of Contents
What is Vasa Previa and How to Manage It
Vasa previa is a rare but serious complication of pregnancy that can endanger the life of your baby. In this blog post, we will explain what vasa previa is, what causes it, how it is diagnosed, and how it is treated.
What is Vasa Previa?
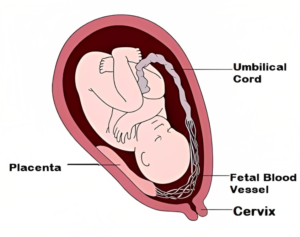
Vasa previa is a condition where some of the blood vessels from the umbilical cord or the placenta cross over or run near the opening of the cervix. These blood vessels are unprotected by the umbilical cord or the placenta tissue and are vulnerable to rupture when the membranes break during labor or delivery. This can cause severe bleeding for the baby and lead to fetal distress, shock, or even death.
Vasa previa affects about 1 in 2,500 pregnancies and is more common in pregnancies that involve:
- A low-lying placenta (placenta previa)
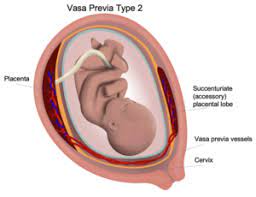
- An abnormal placenta shape (such as a bilobed or succenturiate placenta)
- A velamentous cord insertion (where the umbilical cord attaches to the membranes instead of the placenta)
- In vitro fertilization (IVF)
- Multiple babies
Types of Vasa Previa
There are three types of vasa previa:
Type I: Vasa previa with velamentous cord insertion. In this type, the umbilical cord attaches to the membranes instead of the placenta, and the blood vessels from the cord travel outside the placenta, crossing over or running near the cervix. This type is the most common, accounting for about 90% of cases.
Type II: Vasa previa with a bilobed or succenturiate placenta. This occurs when the placenta is divided into two or more lobes that are connected by blood vessels. The blood vessels between the lobes cross over or run near the cervix.
Type III: Vasa previa with placental atrophy. In this type, a portion of the placenta that covers the cervix degenerates, leaving unprotected blood vessels that cross over or run near the cervix.
Difference Between Vasa Previa Vs Placenta Previa
| Category | Vasa Previa | Placenta Previa |
|---|---|---|
| Definition | Blood vessels from umbilical cord or placenta cross or run near the cervix | Placenta partially or fully covers the cervix |
| Risk of Rupture | Blood vessels are unprotected and vulnerable to rupture during labor or delivery | Placental blood vessels can break and bleed during labor |
| Complications | Severe bleeding, fetal distress, shock, or death | Bleeding, premature labor, difficulty in delivery |
| Prevalence | Approximately 1 in 2,500 pregnancies | Approximately 1 in 200 pregnancies |
| Risk Factors | Low-lying placenta, abnormal placenta shape, velamentous cord insertion, in vitro fertilization, multiple pregnancies | Previous cesarean deliveries, multiple pregnancies, carrying twins or triplets |
| Diagnosis | Transvaginal ultrasound scan with color Doppler during pregnancy | Routine ultrasound scan during pregnancy |
| Treatment | Planned cesarean delivery before labor starts, typically between 34 and 37 weeks of gestation | Planned cesarean delivery before labor starts, usually after 36 weeks of gestation |
How is vasa previa diagnosed?
Vasa previa can be difficult to detect during pregnancy because it often does not cause any symptoms until labor or delivery. However, with routine ultrasound scans and color Doppler imaging, vasa previa can be diagnosed before birth and managed accordingly.
A transvaginal ultrasound scan with color Doppler is the best method to diagnose vasa previa. This involves inserting a probe into the vagina and using sound waves to create an image of the cervix and the blood vessels. The color Doppler helps to distinguish between maternal and fetal blood vessels and to identify any that cross over or run near the cervical opening.
If vasa previa is suspected or confirmed, you will need to have regular monitoring and follow-up scans to check the condition of your baby and the location of the blood vessels. You will also need to avoid any activities that could trigger labor or rupture of membranes, such as sexual intercourse, vaginal exams, or exercise.
How is vasa previa treated?
The main goal of treating vasa previa is to prevent bleeding and deliver your baby safely. The treatment plan will depend on several factors, such as:
- The gestational age of your baby
- The severity of vasa previa
- The presence of any other complications
- Your preferences and values
The most common treatment for vasa previa is a planned cesarean delivery (c-section) before labor starts. This reduces the risk of rupturing the blood vessels and causing fetal hemorrhage. The optimal timing for a c-section delivery varies depending on different studies and guidelines, but it is usually recommended between 34 and 37 weeks of gestation.
In some cases, you may need to have a c-section earlier than planned if you have signs of labor, rupture of membranes, bleeding, or fetal distress. You may also need to have steroid injections to help mature your baby’s lungs and prevent respiratory problems after birth.
In rare cases, you may be able to have a vaginal delivery if vasa previa resolves spontaneously or if the blood vessels are far enough from the cervical opening. However, this option carries a higher risk of complications and requires careful monitoring and preparation.
What are the outcomes of vasa previa?
The outcomes of vasa previa depend largely on whether it is diagnosed before birth and whether appropriate treatment is given. If vasa previa is undiagnosed or untreated, it can result in stillbirth in up to 56% of cases. However, if vasa previa is diagnosed early and managed with a planned c-section delivery, the survival rate for babies can be as high as 97%.
Most babies who survive vasa previa do not have any long-term complications or disabilities. However, some may experience problems such as:
- Anemia (low red blood cell count)
- Hypovolemic shock (low blood volume)
- Hypoxic-ischemic encephalopathy (brain damage due to lack of oxygen)
- Intraventricular hemorrhage (bleeding in the brain)
- Necrotizing enterocolitis (inflammation of the intestines)
- Sepsis (infection in the blood)
These complications are more likely to occur in babies who are born prematurely, have severe bleeding, or have other health issues. Therefore, it is important to monitor your baby closely after birth and provide any necessary interventions or treatments.
How can vasa previa be prevented?
There is no known way to prevent vasa previa from occurring, as it is related to how the placenta and the umbilical cord develop during pregnancy. However, you can reduce the risk of complications and improve the outcomes for your baby by:
- Having regular prenatal care and ultrasound scans
- Seeking medical attention if you have any painless vaginal bleeding
- Following your doctor’s advice on when and how to deliver your baby
- Being aware of the signs of labor, rupture of membranes, and fetal distress
- Having a support system of family, friends, and healthcare professionals
Vasa previa is a rare but serious condition that can have devastating consequences for your baby if it is not diagnosed and treated properly. However, with advances in technology and medical care, most cases of vasa previa can be detected before birth and managed successfully. If you have vasa previa or are at risk of developing it, talk to your doctor about your options and expectations and prepare yourself for safe and healthy delivery.
Nursing Responsibilities in Vasa Previa
The nursing responsibilities in vasa previa include:
- Assisting in the treatment of the disorder by identifying it and providing support. This involves monitoring fetal heart rate and status during labor, assisting in the diagnosis process, and being prepared for emergency cesarean birth.
- Providing physical and emotional support to both the patient and their family. This includes explaining emergency procedures and potential outcomes associated with vasa previa.
- Educating the patient and their family about vasa previa, including its causes, risks, and management. Additionally, discussing the plan for delivery and postpartum care.
- Ensuring regular prenatal care and conducting ultrasound scans to monitor the patient’s condition. Being vigilant for signs of labor, rupture of membranes, bleeding, or fetal distress.
- Administering corticosteroids, if necessary, to aid in the maturation of the baby’s lungs.
References
(1) Vasa praevia – Wikipedia.
(2) Vasa Previa: Causes. Symptoms, Management & Treatment – Cleveland Clinic.
(3) Vasa Previa: Symptoms, Management, and Treatment – Healthline.
FAQs
Q: What is vasa previa?
A: Vasa previa is a condition where the blood vessels from the umbilical cord or placenta cross or run near the opening of the cervix, making them vulnerable to rupture during labor or delivery.
Q: How common is vasa previa?
A: Vasa previa affects approximately 1 in 2,500 pregnancies.
Q: What are the risk factors for vasa previa?
A: Risk factors for vasa previa include a low-lying placenta, an abnormal placenta shape, velamentous cord insertion, in vitro fertilization, or multiple pregnancies.
Q: How is vasa previa diagnosed?
A: Vasa previa can be diagnosed before birth using a transvaginal ultrasound scan with color Doppler.
Q: What are the complications of vasa previa?
A: Vasa previa can cause severe bleeding for the baby, leading to fetal distress, shock, or even death.
Q: What is the treatment for vasa previa?
A: The main treatment for vasa previa is a planned cesarean delivery before labor starts, usually between 34 and 37 weeks of gestation.