Gestational trophoblastic disease (GTD) is a rare condition that occurs during pregnancy and is caused by abnormal growth of cells in the uterus. While it is a relatively uncommon condition, it is important for women to understand the symptoms, diagnosis, and treatment options associated with GTD.
Table of Contents
What is Gestational Trophoblastic Disease?
Gestational Trophoblastic Disease (GTD) is a rare condition that develops during pregnancy. It occurs when there is an overgrowth of cells that help form the placenta. These cells are called trophoblastic cells, and they can multiply abnormally, leading to several types of tumors.
Signs and Symptoms
Signs and symptoms of Gestational Trophoblastic Disease (GTD) may include:
- Vaginal bleeding
- Abnormally high levels of human chorionic gonadotropin (hCG) in the blood
- Presence of abnormal cysts or tumors in the uterus
- Nausea
- Vomiting
- Abdominal pain
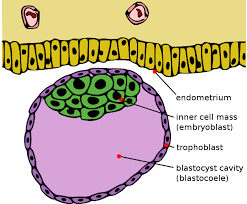
The Role of Trophoblastic Cells in Pregnancy
Trophoblastic cells are the cells that form the outer layer of the blastocyst, which is the fertilized egg that implants in the uterus. These cells eventually form the placenta, which provides nutrients and oxygen to the developing fetus. In most pregnancies, the trophoblastic cells develop normally, but in some cases, they can develop abnormally, leading to GTD.
Types of Gestational Trophoblastic Disease
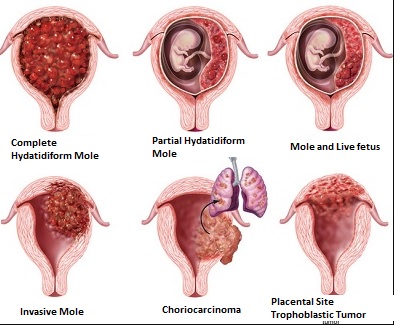
1. Complete Hydatidiform Mole
Complete hydatidiform mole, also known as a complete molar pregnancy, occurs when all the genetic material in the fertilized egg comes from the father. This results in the absence of a viable fetus, and instead, the placenta grows abnormally, resembling a cluster of grapes.
2. Partial Hydatidiform Mole
A partial hydatidiform mole occurs when there is an abnormal combination of genetic material from both the mother and the father. This condition can result in the growth of some fetal tissue, but it is typically nonviable.
3. Invasive Mole
Invasive mole is a rare type of molar pregnancy that occurs when the trophoblastic cells invade the muscle tissue of the uterus. This condition is not cancerous, but it can cause significant bleeding and damage to the uterus.
4. Choriocarcinoma
Choriocarcinoma is rare cancer that can develop after a molar pregnancy or a normal pregnancy. It occurs when the trophoblastic cells become cancerous and can spread to other parts of the body.
5. Placental Site Trophoblastic Tumor
Placental site trophoblastic tumor is a rare type of GTD that occurs after a normal pregnancy. It develops when the trophoblastic cells that form the site of the placenta continue to grow abnormally after delivery.
Causes and Risk Factors Associated with Gestational Trophoblastic Disease
a. Hormonal Factors
Hormonal imbalances during pregnancy can lead to abnormal growth of trophoblastic cells and increase the risk of GTD. Women who have hormonal disorders, such as polycystic ovary syndrome, are at higher risk for developing GTD.
b. Genetic Factors
Abnormalities in the genetic material of the fertilized egg, such as having an extra set of chromosomes, can increase the risk of GTD.
c. Age and Pregnancy History
Women who are younger than 20 or older than 40 are at higher risk for developing GTD. Additionally, women who have had multiple pregnancies are at higher risk as well.
d. Environmental Factors
Exposure to certain environmental toxins, such as pesticides, can increase the risk of GTD.
Diagnosis of Gestational Trophoblastic Disease
The diagnosis of GTD can vary depending on the type. Diagnostic tests for GTD may include
- physical exam
- blood tests
- ultrasound
- imaging tests
- A biopsy may also be performed to confirm a diagnosis.
Distinguishing Gestational Trophoblastic Disease from Other Conditions
GTD can be mistaken for other conditions, such as miscarriage or ectopic pregnancy. A thorough medical evaluation and diagnostic testing can help distinguish GTD from other conditions.
Complications of Gestational Trophoblastic Disease
Here are some of the complications of Gestational Trophoblastic Disease:
- Persistent Gestational Trophoblastic Neoplasia (GTN)
- Choriocarcinoma
- Placental Site Trophoblastic Tumor (PSTT)
- Uterine Rupture
- Pulmonary Embolism
- Hemorrhage
- Ovarian Hyperstimulation Syndrome (OHSS)
- Thyroid dysfunction
- Chemotherapy-related complications
- Infertility
It is important to note that not all women with GTD will experience these complications, and prompt diagnosis and treatment can greatly reduce the risk of complications.
Treatment Options for Gestational Trophoblastic Disease
GTD develops when abnormal cells form in the tissues that would normally become the placenta during pregnancy. Treatment options for GTD depend on its severity, and usually include one or more of the following:
i. Surgical Treatment
In many cases, this can be done through a procedure called dilation and curettage (D&C). In cases of severe GTD, surgery may be necessary to remove the cancerous tissues. This may involve a hysterectomy (removal of the uterus), or a less invasive procedure in which only the placenta and other affected tissues are removed.
ii. Chemotherapy
Chemotherapy involves using drugs to kill cancer cells. This treatment is often used to treat GTD, even if the disease has not spread beyond the uterus. The length and type of chemotherapy treatment vary depending on the severity of the disease.
iii. Radiation Therapy
Radiation therapy may be used in cases where GTD has spread. This treatment involves using high-energy X-rays to kill cancer cells. Radiation therapy is typically used in combination with chemotherapy or after surgery.
iv. Combined Modality Therapy
Combined modality therapy involves using more than one type of treatment (such as surgery, chemotherapy, and radiation therapy) to treat GTD. This approach is often used for more advanced cases of the disease.
Recovery and Follow-up Care for Gestational Trophoblastic Disease
After successful treatment, most women with GTD can go on to have healthy pregnancies. However, it is essential to monitor them closely with follow-up care, including regular check-ups and testing.
Recovery Time and Follow-up Tests
The recovery time for women with GTD depends on the severity of the disease and the type of treatment they received. After treatment, patients will require regular follow-up tests, including blood tests, imaging studies, and physical exams. These tests are crucial to ensure the disease does not return.
Long-term Health Considerations
Women with GTD may be at an increased risk of developing certain health problems later in life, such as high blood pressure and thyroid disease. Regular monitoring and checkups can catch these issues early, allowing for timely treatment.
Nursing Responsibilities
As a nursing professional, it is crucial to provide high-quality care to patients with Gestational Trophoblastic Disease (GTD). Here are some nursing responsibilities that can help improve the patient’s outcomes:
- Monitor vital signs: It is important to monitor the patient’s vital signs frequently, including blood pressure, heart rate, and respiratory rate, to ensure that they remain stable.
- Assess bleeding and fluid loss: GTD often leads to vaginal bleeding and fluid loss, which can lead to dehydration and electrolyte imbalances. Nurses should assess and monitor the amount and color of vaginal bleeding, urine output, and electrolyte levels regularly.
- Administer medication: Patients with GTD may require medications to manage their symptoms, prevent infection, and promote healing. Nurses should administer medications as prescribed, monitor for adverse effects, and educate patients about their medication regimen.
- Provide emotional support: Diagnosis of GTD can be stressful and emotional for patients and their families. Nurses should provide emotional support, offer counseling services, and connect patients with support groups or other resources to help them cope with their diagnosis.
- Educate patients about self-care: It is important to educate patients about self-care, including proper nutrition, hydration, and rest. Nurses should also instruct patients on how to monitor their symptoms and when to seek medical attention.
- Collaborate with the healthcare team: Nurses should collaborate with the healthcare team, including physicians, social workers, and other healthcare professionals, to ensure comprehensive care for patients with GTD.
- Monitor for complications: GTD can lead to several complications, including hemorrhage, infection, and malignancy. Nurses should monitor for signs and symptoms of complications and promptly report any concerns to the healthcare team.
Emotional Support for Women with Gestational Trophoblastic Disease
A diagnosis of GTD can be overwhelming and emotional. Women with GTD may require additional emotional support to help them cope with their diagnosis and treatment.
Coping Strategies
Coping strategies can include seeking counseling or therapy to help manage anxiety or depression. Talking to friends and family members can also provide emotional support and help alleviate feelings of isolation.
Patient Support Groups
Joining a support group of other women who have experienced GTD can be an excellent source of support and encouragement. These groups can provide a safe space to share feelings, ask questions, and learn coping strategies from others who have been through similar experiences. The gestational trophoblastic disease can be a difficult condition to experience, but with early diagnosis and appropriate treatment, most women can make a full recovery.
Follow-up care and emotional support can also be instrumental in helping women navigate the recovery process. If you are experiencing symptoms associated with GTD, it’s important to speak with your healthcare provider right away to receive proper care and support.
FAQs About Gestational Trophoblastic Disease
Q: What is Gestational Trophoblastic Disease (GTD)?
A: Gestational Trophoblastic Disease (GTD) is a group of rare pregnancy-related disorders that arise from abnormal growth of trophoblastic cells, which are the cells that normally develop into the placenta.
Q: What are the different types of GTD?
A: There are several types of GTD, including complete hydatidiform mole (CHM), partial hydatidiform mole (PHM), invasive mole, choriocarcinoma, and placental site trophoblastic tumor (PSTT).
Q: What are the symptoms of GTD?
A: The signs and symptoms of GTD can vary depending on the type of disease, but they often include vaginal bleeding, abnormally high levels of human chorionic gonadotropin (hCG) in the blood, and the presence of abnormal cysts or tumors in the uterus. GTD can also cause other symptoms such as nausea, vomiting, and abdominal pain.
Q: What are the risk factors for GTD?
A: Women who are younger than 20 or older than 35, women who have a history of GTD, and women who have had multiple pregnancies are at a higher risk of developing GTD.
Q: How is GTD diagnosed?
A: GTD is typically diagnosed through a combination of a physical exam, imaging tests (such as ultrasound), and blood tests to measure hCG levels.
Q: How is GTD treated?
A: The treatment for GTD depends on the type and stage of the disease. Treatment options may include surgery, chemotherapy, and/or radiation therapy.
Q: What is the prognosis for GTD?
A: Most cases of GTD can be successfully treated, and the prognosis is generally very good. However, it is important to closely monitor hCG levels after treatment to ensure that the disease does not recur.
Is Gestational Trophoblastic Disease Common?
No, gestational trophoblastic disease is a rare condition that occurs in about 1 in every 1000 pregnancies.
Can Gestational Trophoblastic Disease Cause Cancer?
In some cases, gestational trophoblastic disease can develop into a type of cancer called choriocarcinoma. However, with appropriate treatment, most women can make a full recovery.
Can Gestational Trophoblastic Disease Affect Future Pregnancies?
Women who have had gestational trophoblastic disease may have a slightly increased risk of developing it again in future pregnancies. However, the overall risk is still low, and most women are able to go on to have healthy pregnancies.
What Emotional Support is Available for Women with Gestational Trophoblastic Disease?
Many women find it helpful to connect with support groups or counselors who specialize in pregnancy-related health issues. Your healthcare provider can help you find support resources in your community.
Latest Posts
- NVS Staff Nurse Vacancy 2024 – How to Apply

- AIIMS NORCET 6 and ESIC Nursing Exam Questions and Answers


- ESIC Nursing Officer Recruitment 2024 | 1930 Vacancies – Apply Now



- Dream Job Alert: AIIMS NORCET Nursing Officer Vacancy 2024 – Apply Now!



- NIMHANS Nursing Officer Exam 17-12-2023 Memory-Based Solved Questions