Table of Contents
How to Recognize Digoxin Toxicity EKG Findings
Digoxin is a medication that is used to treat heart failure and certain types of arrhythmias. It works by increasing the force and efficiency of the heart contractions, and by slowing down the electrical impulses that cause irregular heartbeats.
However, digoxin can also cause serious side effects if the dose is too high or if the patient has other risk factors, such as kidney problems, electrolyte imbalances, or drug interactions. Digoxin toxicity can affect various organs and systems, but the most common and dangerous manifestation is cardiac toxicity, which can lead to life-threatening arrhythmias and cardiac arrest.
One of the best ways to diagnose and monitor digoxin toxicity is by using an electrocardiogram (EKG), which is a test that records the electrical activity of the heart. Digoxin toxicity can cause characteristic EKG changes that can help clinicians identify and treat this condition.
We will explain how to recognize digoxin toxicity EKG findings, what are the different types and subtypes of digoxin toxicity EKG changes, and some tips and guidelines to follow when interpreting an EKG for digoxin toxicity.
How to Recognize Digoxin Toxicity EKG Findings
The EKG findings of digoxin toxicity can be divided into two main categories:
- Digoxin effect: This refers to the normal EKG changes that occur with therapeutic doses of digoxin. It does not indicate toxicity but rather shows that the patient is taking digoxin. The digoxin effect can be seen as:
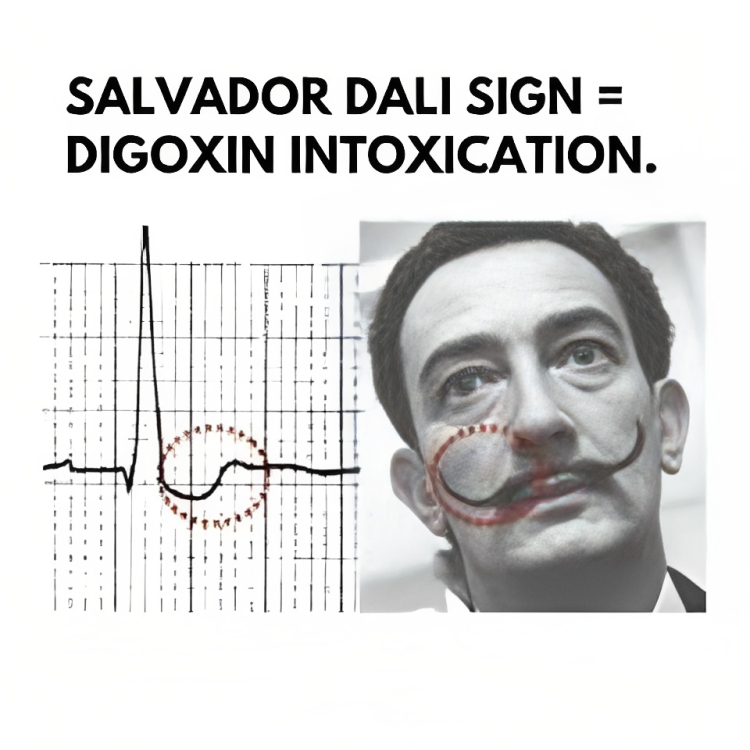
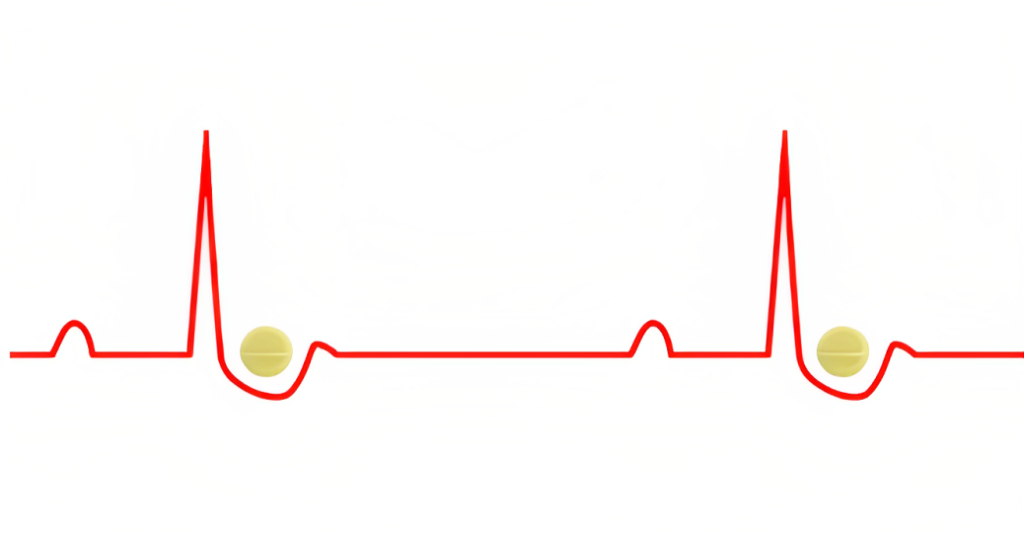
- Downsloping ST segment depression with a characteristic “scooped out” or “Salvador Dali sagging” appearance
- Flattened, inverted, or biphasic T waves
- Shortened QT interval
- Mild PR interval prolongation (up to 240 ms) due to increased vagal tone at the AV node
- Prominent U waves
- Peaking of the terminal portion of the T waves
- J point depression (usually in leads with tall R waves)
- Digoxin toxicity: This refers to abnormal EKG changes that occur with excessive doses of digoxin or with other factors that increase its level or effect. It indicates cardiac toxicity and requires urgent treatment. Digoxin toxicity can be seen as:
- Signs of increased automaticity (increased intracellular calcium) such as:
- Frequent premature ventricular contractions (PVCs), which are the most common and earliest arrhythmia
- Ventricular tachycardia (VT), including polymorphic and bidirectional VT
- Ventricular fibrillation (VF)
- Atrial tachycardia (AT) or atrial fibrillation (AF) with a fast ventricular rate
- Signs of decreased AV conduction (increased vagal effects at the AV node) such as:
- Sinus bradycardia
- Any type of AV block (1st degree, 2nd degree, or 3rd degree)
- Paroxysmal atrial tachycardia with a block (PAT with block)
- Regularized AF (AF with complete heart block and a junctional or ventricular escape rhythm)
- Signs of increased automaticity (increased intracellular calcium) such as:
The most classic EKG pattern of digoxin toxicity is a combination of supraventricular tachycardia (SVT) with a slow ventricular response due to AV block. However, any type of arrhythmia can occur with digoxin toxicity, and some patients may have normal sinus rhythm despite having high levels of digoxin.
Therefore, it is important to correlate the EKG findings with the clinical features, history of digoxin intake, history of other illnesses, and serum digoxin levels.
How To Recognize Digoxin Toxicity EKG Easily

When interpreting an EKG for digoxin toxicity, it is important to follow these tips and guidelines:
- Compare the current EKG with previous EKGs to look for any new or worsening changes.
- Look for signs of digoxin effect in all leads, especially in leads with dominant R waves (V4-V6, I, aVL).
- Look for signs of digoxin toxicity in all leads, especially in leads with dominant S waves (V1-V3).
- Consider other causes of similar EKG changes, such as ischemia, electrolyte imbalances, or drug interactions.
- Consider the possibility of digoxin toxicity even if the patient has normal sinus rhythm or normal serum digoxin levels, as these may not reflect the true tissue level or effect of digoxin.
- Consult a cardiologist or a toxicologist if in doubt or if the patient has severe or refractory arrhythmias.
Normal values of serum digoxin level:
The therapeutic range for serum digoxin level varies but is generally considered to be 0.5 to 2.0 nanograms per milliliter (ng/mL) for adults. However, it’s important to note that optimal therapeutic levels may vary depending on the patient’s condition and individual factors. Close monitoring of serum digoxin levels is essential to ensure safe and effective use.
The recommended dose of digoxin:
The recommended dose of digoxin depends on the patient’s age, weight, renal function, and the condition being treated. The dosing is typically individualized for each patient. It’s important to follow the prescribed dose and regimen provided by the healthcare provider.
Causes of digoxin toxicity:
- Overdose: Taking a higher dose of digoxin than prescribed or recommended.
- Drug interactions: Certain medications, such as verapamil, amiodarone, or quinidine, can increase digoxin levels and the risk of toxicity.
- Renal impairment: Impaired kidney function can lead to decreased elimination of digoxin from the body, resulting in higher levels.
- Hypokalemia: Low levels of potassium in the blood can enhance the toxicity of digoxin.
- Advanced age: Older adults may be more susceptible to digoxin toxicity due to age-related changes in drug metabolism and clearance.
Signs and symptoms of digoxin toxicity:
- Nausea, vomiting, and loss of appetite.
- Arrhythmias or irregular heartbeat.
- Visual disturbances, such as blurred or yellow-tinged vision, or seeing halos around objects.
- Fatigue, weakness, or confusion.
- Dizziness or fainting.
- Abdominal pain.
Treatment of digoxin toxicity:
- Discontinuation of digoxin: Stopping the administration of digoxin to prevent further toxicity.
- Activated charcoal: Administered to absorb any remaining digoxin in cases of a recent overdose.
- Digoxin-specific antibody fragments: These are used in severe cases of toxicity to bind to digoxin and facilitate its elimination from the body. Eg: Digibind
- Supportive care: Monitoring vital signs, electrolyte levels, and cardiac function. Treatment of arrhythmias or electrolyte imbalances if present.
Complications of digoxin toxicity:
- Life-threatening arrhythmias, such as ventricular tachycardia or fibrillation.
- Cardiac arrest.
- Multiorgan dysfunction or failure.
Prevention of digoxin toxicity:
- Follow prescribed dosages: Take digoxin as directed by the healthcare provider and avoid exceeding the recommended dose.
- Regular monitoring: Regularly monitor serum digoxin levels to ensure they are within the therapeutic range.
- Report any new symptoms: Notify the healthcare provider promptly if experiencing any new or worsening symptoms while taking digoxin.
- Inform healthcare providers: Inform all healthcare providers about current digoxin use to avoid potential drug interactions.
- Maintain a healthy lifestyle: Follow a balanced diet, exercise regularly, and avoid excessive alcohol consumption to promote overall cardiovascular health.
Nursing Responsibilities
Nursing responsibilities in cases of digoxin toxicity include:
- Monitoring vital signs: Regularly assess and monitor the patient’s blood pressure, heart rate, and respiratory rate. Changes in vital signs can indicate worsening toxicity or complications.
- Assessing cardiac rhythm: Perform continuous cardiac monitoring to identify any abnormal rhythms or arrhythmias. Monitor for signs of bradycardia, tachycardia, or irregular heartbeat.
- Monitoring electrolyte levels: Check serum potassium levels, as low potassium levels can increase the risk of digoxin toxicity. Assess other electrolyte levels, such as calcium and magnesium, as imbalances can affect cardiac function.
- Evaluating clinical symptoms: Assess the patient for signs and symptoms of digoxin toxicity, such as nausea, vomiting, changes in vision, confusion, weakness, and arrhythmias. Document and report any observed changes promptly.
- Medication administration: Administer medications as prescribed by the healthcare provider, which may include administering digoxin-specific antibody fragments (Digibind) in severe cases of toxicity.
- Providing patient education: Educate the patient and their family about the signs and symptoms of digoxin toxicity, the importance of adhering to prescribed dosages, and when to seek medical assistance.
- Collaborating with the healthcare team: Communicate and collaborate with the healthcare team, including physicians, pharmacists, and other nurses, to ensure appropriate monitoring, management, and treatment of digoxin toxicity.
- Documenting findings: Accurately document the patient’s vital signs, symptoms, medication administration, and any interventions or changes in condition. Maintain clear and concise documentation to facilitate communication and continuity of care.
- Promoting patient safety: Ensure a safe environment for the patient, including fall precautions, as digoxin toxicity can cause dizziness and balance disturbances.
- Continual assessment and evaluation: Regularly reassess the patient’s response to treatment and monitor for any improvement or worsening of symptoms. Adjust nursing care accordingly and communicate changes to the healthcare team.
It’s important for nurses to stay updated on the latest evidence-based practices and guidelines related to digoxin toxicity management and to consult with the healthcare team for specific protocols and interventions.
Conclusion
Digoxin toxicity is a serious condition that can cause fatal cardiac arrhythmias. EKG is a valuable tool to diagnose and monitor digoxin toxicity, as it can show characteristic changes that reflect the effect and toxicity of digoxin on the heart.
I hope this blog post helps you understand how to recognize digoxin toxicity EKG findings and what are the different types and subtypes of digoxin toxicity EKG changes. If you have any questions or feedback, please contact us. Thank you for reading! 💓
References
(1) Digoxin toxicity – Wikipedia.
(2) Digoxin Toxicity • LITFL • ECG Library Toxicology.
(3) Digoxin Toxicity | ECG Disease Patterns – MedSchool.
(4) Digoxin toxicity – Symptoms, diagnosis and treatment – BMJ Best Practice.
FAQs: Digoxin Toxicity EKG Findings
Q1: What are the EKG findings commonly seen in digoxin toxicity?
A1: Digoxin toxicity can produce various EKG findings, including bradyarrhythmias (such as sinus bradycardia or atrioventricular block), tachyarrhythmias (such as atrial tachycardia or atrial fibrillation with slow ventricular response), and ST segment and T wave changes (such as scooping or flattening of ST segments and inverted or biphasic T waves).
Q2: Can digoxin toxicity cause bradycardia on an EKG?
A2: Yes, digoxin toxicity can cause bradycardia, and it is one of the common EKG findings associated with digoxin toxicity. Sinus bradycardia or atrioventricular block may be observed.
Q3: Are tachyarrhythmias common in digoxin toxicity EKG findings?
A3: Yes, tachyarrhythmias are also frequently seen in digoxin toxicity. Atrial tachycardia and atrial fibrillation with a slow ventricular response are common manifestations.
Q4: What are the ST segment and T wave changes seen in digoxin toxicity on an EKG?
A4: Digoxin toxicity can cause ST segment depression, especially in the downsloping or scooping pattern, as well as T wave inversion or biphasic T waves. These changes are often observed in multiple leads.
Q5: Can EKG findings alone confirm digoxin toxicity?
A5: EKG findings alone cannot definitively confirm digoxin toxicity. They provide valuable information, but a comprehensive assessment that includes clinical symptoms, serum digoxin levels, and patient history is necessary for an accurate diagnosis.
Q6: Are there specific EKG criteria for diagnosing digoxin toxicity?
A6: While there are no specific EKG criteria that can solely diagnose digoxin toxicity, certain EKG patterns, such as atrial tachycardia with AV block or atrial fibrillation with a slow ventricular response, can raise suspicion for digoxin toxicity. The diagnosis is confirmed through a combination of clinical evaluation and laboratory testing.
Q7: How should healthcare providers interpret EKG findings in suspected cases of digoxin toxicity?
A7: EKG findings should be evaluated in the context of the patient’s clinical presentation and digoxin levels. If there are concerning EKG changes along with symptoms suggestive of digoxin toxicity, further investigation, such as serum digoxin level measurement, is warranted.
Q8: Can other conditions or medications cause similar EKG changes as digoxin toxicity?
A8: Yes, other conditions and medications can produce EKG changes similar to those seen in digoxin toxicity. Differential diagnosis should consider electrolyte imbalances, other antiarrhythmic medications, myocardial ischemia, and structural heart disease.
Q9: How can healthcare providers differentiate between digoxin toxicity and other causes of EKG abnormalities?
A9: Differentiation requires a thorough evaluation that includes patient history, medication reconciliation, physical examination, laboratory tests (including serum digoxin levels), and consideration of other potential causes for EKG abnormalities.
Q10: Can EKG findings guide treatment decisions for digoxin toxicity?
A10: EKG findings, along with clinical presentation and laboratory results, contribute to the overall assessment of digoxin toxicity. They assist healthcare providers in determining appropriate management strategies, but treatment decisions are based on the complete clinical picture.