A uterine fibroid that grows on the outside of the uterus is known as a subserosal fibroid. Uterine fibroids are noncancerous tumors that grow from the uterus’ smooth muscle cells. They are extremely frequent, affecting up to 80% of women by the age of 50.
The size, form, and number of subserosal fibroids might vary. They might be directly linked to the uterus or via a thin stalk known as a pedunculated fibroid. They can grow on any area of the uterus’s exterior surface and can sometimes spread to adjacent organs such as the bladder or colon.
Subserosal fibroids are mostly noncancerous and do not increase the risk of uterine cancer. They can, however, induce symptoms and consequences that have an impact on your quality of life and health. We will examine what causes subserosal fibroids, how they are diagnosed, what symptoms they can cause, and what treatment options are available in this blog post.
Table of Contents
Types of Subserosal Fibroids
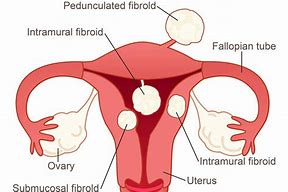
There are several types of subserosal fibroids, which are differentiated based on their location and size. These types include:
- Pedunculated subserosal fibroids: These fibroids are attached to the uterus by a stalk or stem and can protrude into the abdominal cavity.
- Broad-based subserosal fibroids: These fibroids are attached to the uterus over a larger area and tend to be flatter and wider than pedunculated subserosal fibroids.
- Intraligamentous subserosal fibroids: These fibroids grow within the ligaments that support the uterus, rather than directly on the uterus itself.
- Anterior subserosal fibroids: These fibroids grow on the front of the uterus, towards the abdominal cavity.
- Posterior subserosal fibroids: These fibroids grow on the back of the uterus, towards the spinal cord.
Pedunculated Subserosal Fibroid
A pedunculated subserosal fibroid is a type of subserosal fibroid that is attached to the uterus by a stalk or stem and protrudes into the abdominal cavity. These fibroids can vary in size and may grow to be quite large, causing discomfort and pain. Symptoms of pedunculated subserosal fibroids can include pelvic pain or pressure, heavy menstrual bleeding, frequent urination, and constipation.
In some cases, the fibroid may become twisted on its stalk, cutting off its blood supply and causing severe pain, and potentially requiring emergency medical attention. Treatment options for pedunculated subserosal fibroids may include medication to manage symptoms, minimally invasive procedures such as laparoscopic or robotic surgery to remove the fibroid, or hysterectomy in more severe cases.
Broad-based subserosal fibroids
Broad-based subserosal fibroids are a type of subserosal fibroid that is attached to the uterus over a larger area than a pedunculated subserosal fibroid. These fibroids are typically flatter and wider than pedunculated subserosal fibroids and can grow to be quite large. Broad-based subserosal fibroids may cause discomfort and pain, as well as symptoms such as pelvic pressure, bloating, and back pain. In some cases, they may also cause heavy menstrual bleeding, frequent urination, and constipation.
Intraligamentous subserosal fibroids
Intraligamentous subserosal fibroids are a type of subserosal fibroid that grows within the broad ligament of the uterus, which is the sheet of tissue that supports the uterus in the pelvic cavity. These fibroids can grow to be quite large and may cause pelvic pain or pressure, as well as symptoms such as frequent urination and constipation. Intraligamentous subserosal fibroids may also cause abnormal vaginal bleeding or spotting between periods.
Subserosal Fibroid in Anterior Wall
A subserosal fibroid in the anterior wall of the uterus is a type of fibroid that grows on the outside of the uterus, towards the front of the body. While the location of the fibroid may not affect its overall impact on the body, an anterior subserosal fibroid may cause more visible or noticeable symptoms.
For example, if the fibroid grows large enough, it may cause a noticeable bulge in the lower abdomen or pelvis. Other symptoms of an anterior subserosal fibroid may include pelvic pain or pressure, pain during sex, back pain, and heavy menstrual bleeding. Treatment options for this type of fibroid may include medications to manage symptoms or surgery to remove the fibroid altogether.
Posterior subserosal fibroids
Posterior subserosal fibroids are a type of subserosal fibroid that grows on the back or posterior surface of the uterus and protrudes into the abdominal cavity. These fibroids can vary in size and may cause discomfort and pain, as well as symptoms such as pelvic pressure, back pain, and constipation. Posterior subserosal fibroids may also cause heavy menstrual bleeding, frequent urination, and difficulty emptying the bladder.
What Causes Subserosal Fibroids?
Although the particular cause of subserosal fibroids is unknown, experts believe that a number of factors may play a role in their formation. These are some examples:
Genetic Changes: Subserosal fibroids may have abnormalities in their DNA that distinguish them from normal uterine muscle cells. These alterations could have an impact on how they grow and respond to hormones.
Hormones: Subserosal fibroids are sensitive to the hormones estrogen and progesterone, which govern the menstrual cycle and pregnancy. During the reproductive years, these hormones may induce the growth of subserosal fibroids, which may diminish following menopause.
Growth factors: Subserosal fibroids can create or respond to growth hormones such as insulin-like growth factor (IGF) and vascular endothelial growth factor (VEGF). These factors may help subserosal fibroids grow larger and obtain more blood flow.
Inflammation: Chronic inflammation in the pelvic region, which can be caused by infections, traumas, or autoimmune illnesses, might influence subserosal fibroids. Inflammation can cause the production of substances that promote cell development and the creation of blood vessels.
Risk Factors
Age: Subserosal fibroids are more common in adults in their 30s and 40s, and less common in people under the age of 20 or above the age of 50.
Ethnicity: Subserosal fibroids are more common among African-Americans than among Whites or other ethnic groups. Black people also have a higher risk of developing subserosal fibroids at a younger age, larger and more numerous subserosal fibroids, and more severe symptoms and problems.
Family history: Subserosal fibroids are known to run in families. You are more prone to get subserosal fibroids if you have a parent or sibling who has them.
Obesity: Subserosal fibroids are more common in overweight or obese people than in normal-weight people. Obesity may raise estrogen and inflammatory levels in the body, promoting subserosal fibroid growth.
Diet: Your food habits may have an impact on subserosal fibroids. Consuming a lot of red meat, processed foods, alcohol, or caffeine may increase your risk, whereas eating more fruits, vegetables, whole grains, legumes, fish, or dairy products may lessen your risk.
Reproductive history: Subserosal fibroids may be affected by your reproductive history. Having an early onset of menstruation (before age 10), having no or few pregnancies, having a late onset of menopause (after age 55), or using oral contraceptives for a long time may increase your risk of subserosal fibroids, while having multiple pregnancies or breastfeeding for a long time may lower your risk
Subserosal Fibroids with Cystic Degeneration
In some cases, subserosal fibroids may undergo cystic degeneration, a process where the center of the fibroid breaks down and forms a fluid-filled cavity.
Subserosal fibroids with cystic degeneration are a type of uterine fibroid that can cause a variety of symptoms. While the exact cause of this type of fibroid is unknown, research suggests that it may be related to a decrease in blood supply to the fibroid. This can cause the fibroid to break down and form a fluid-filled cavity, which can then lead to cystic degeneration.
In addition to a decrease in blood supply, hormonal imbalances, and genetics may also play a role in the development of subserosal fibroids with cystic degeneration. Hormonal imbalances can cause the uterus to grow larger, which can increase the risk of fibroids. Genetics may also be a factor, as women with a family history of fibroids are more likely to develop them themselves.
Symptoms of subserosal fibroids with cystic degeneration can vary depending on the size and location of the fibroids. While some women may not experience any symptoms at all, others may experience pelvic pain or pressure, bloating or swelling in the abdomen, back pain, pain during sex, heavy menstrual bleeding, urinary frequency or urgency, and difficulty emptying the bladder. In some cases, cystic degeneration can cause acute pain and require emergency medical attention.
How Are Subserosal Fibroids Diagnosed?
Subserosal fibroids may not cause any symptoms and may be discovered incidentally during a routine pelvic exam or an imaging test for another reason. However, if you have symptoms that suggest subserosal fibroids, your doctor may perform one or more of the following tests:
Ultrasound: This is a painless and non-invasive procedure that uses sound waves to make images of your uterus and other pelvic organs. Ultrasound can aid in the detection of subserosal fibroids by determining their presence, size, number, and location. It can also aid in ruling out other potential causes of your symptoms, such as ovarian cysts or endometriosis.
Angiography and Dopplerography: These are ultrasound techniques that focus on the blood arteries that supply the uterus and fibroids. They can assist examine the fibroids’ blood flow and oxygenation, which may affect their growth and response to treatment.
Tomography: This is a form of imaging technique that creates comprehensive cross-sectional images of your uterus and other pelvic organs using X-rays, magnetic fields, or radio waves. Tomography can assist discover subserosal fibroids that are either small or too deep for an ultrasound to detect. It can also assist in determining the effect of subserosal fibroids on neighboring organs such as the bladder or colon.
Laparoscopy: This is a minimally invasive surgical procedure that includes inserting a thin tube (laparoscope) with a camera and light through a small incision in your abdomen. Laparoscopy can help you see the outside of your uterus and confirm the presence of subserosal fibroids. It can also be used to perform a biopsy (taking a small sample of tissue) or a myomectomy (removing the fibroids).
Impact of Subserosal Fibroids During Pregnancy
Subserosal fibroids typically do not affect pregnancy outcomes and often do not cause any symptoms during pregnancy. However, in some cases, subserosal fibroids can cause complications such as:
- Pain: Large subserosal fibroids can cause abdominal or back pain during pregnancy.
- Preterm Labor: Subserosal fibroids can cause the uterus to contract prematurely, leading to preterm labor.
- Placental Abruption: Subserosal fibroids can increase the risk of placental abruption, a condition where the placenta separates from the uterine wall before delivery.
- Fetal Malposition: Subserosal fibroids can sometimes prevent the fetus from assuming the correct position for delivery, such as a head-down position.
How Are Subserosal Fibroids Treated?
The treatment of subserosal fibroids depends on several factors, such as your age, your symptoms, your desire to preserve fertility, the size and number of your fibroids, and your personal preferences. Some possible treatment options include:
Watchful waiting: This means monitoring your condition without any active treatment. This may be an option if you have no or mild symptoms, if you are close to menopause, or if you have small or slow-growing fibroids. You will need regular check-ups and imaging tests to make sure your fibroids do not grow larger or cause complications.
Hormonal therapy: This involves taking medications that affect the levels or actions of estrogen and progesterone in your body. Hormonal therapy can help reduce the bleeding and pain caused by subserosal fibroids, but it does not shrink them significantly or permanently. Hormonal therapy may also have side effects, such as weight gain, mood changes, headaches, nausea, breast tenderness, or irregular bleeding. Hormonal therapy is not recommended if you are trying to get pregnant or if you have a history of blood clots, liver disease, or breast cancer.
Non-hormonal therapy: It entails taking drugs that have no effect on your hormones but can help alleviate some of the symptoms of subserosal fibroids. Nonsteroidal anti-inflammatory drugs (NSAIDs) can, for example, help reduce inflammation and pain; iron supplements can help prevent or treat anemia caused by heavy bleeding; tranexamic acid can help reduce bleeding by preventing blood clots from breaking down; and gonadotropin-releasing hormone (GnRH) antagonists can help block estrogen and progesterone production and temporarily shrink fibroids before surgery. Non-hormonal therapy may also cause stomach upset, bleeding issues, heat flashes, bone loss, or allergic responses.
Myomectomy: This is a surgical procedure that involves removing the fibroids while preserving the uterus. Depending on the size, number, and location of the fibroids, myomectomy can be performed using various techniques such as laparoscopy, hysteroscopy, or laparotomy. Myomectomy can help reduce symptoms of subserosal fibroids while still preserving fertility. Risks of myomectomy include bleeding, infection, scarring, recurrence of fibroids, and harm to surrounding organs. Myomectomy is not advised if you have several or large fibroids or if you do not want to become pregnant in the near future.
What Are Some Alternative Treatments for Subserosal Fibroids?
Some people may prefer to try some natural or alternative treatments for subserosal fibroids, either alone or in combination with conventional treatments. However, the evidence for the effectiveness and safety of these treatments is limited or lacking, so you should always consult your doctor before using them. Some possible alternative treatments for subserosal fibroids include:
Acupuncture: This is a traditional Chinese medicine method in which fine needles are inserted into certain places on your body to stimulate the flow of energy (qi) and blood. Subserosal fibroids can cause inflammation, pain, and bleeding, which acupuncture can help with. More research, however, is required to determine its benefits and hazards.
Exercise: Physical activities that boost your cardiovascular health, strength, flexibility, and mood are included in this category. By lowering estrogen levels, boosting blood circulation, reducing stress, and keeping a healthy weight, exercise may help minimize the risk and symptoms of subserosal fibroids. Exercises that put too much strain on your abdomen or pelvis, such as sit-ups or crunches, should be avoided.
Massage: This is the application of pressure and movement to your muscles and soft tissues in order to relax them and enhance blood flow. Massage may aid in the relief of pain, cramping, and stress caused by subserosal fibroids. Massage should be avoided if you have significant bleeding, infection, or inflammation in your pelvic area.
Herbs: They are plants or plant extracts that are used to cure various health issues. Turmeric, green tea, ginger, chaste berry, milk thistle, and dandelion are some herbs that may have anti-inflammatory, anti-proliferative, or hormone-balancing effects on subserosal fibroids. However, the FDA does not monitor the quality and safety of herbal products, and certain herbs may interact with pharmaceuticals or induce allergic responses. As a result, before using any herbs for subserosal fibroids, you should visit your doctor.
Diet: This involves eating foods that nourish your body and support your hormonal balance. Some dietary changes that may help prevent or treat subserosal fibroids include increasing your intake of fruits, vegetables, whole grains, legumes, fish, and dairy products; reducing your intake of red meat, processed foods, alcohol, and caffeine; and supplementing with vitamin D if you are deficient. However, more research is needed to establish the link between diet and subserosal fibroids.
Subserosal Fibroid and Fertility
Subserosal fibroids can affect fertility in some women, depending on their size, location, and number. While subserosal fibroids are not typically located within the uterine cavity where a fertilized egg implants and grows, they can still impact fertility by altering the shape of the uterus or compressing nearby fallopian tubes. If a subserosal fibroid is located near the fallopian tubes, it may cause blockages or prevent the egg from being released properly.
Additionally, larger subserosal fibroids can cause a noticeable bulge in the lower abdomen, which may impact sexual function or cause discomfort during intercourse. Treatment options for subserosal fibroids and fertility may include surgery to remove the fibroid, medication to manage symptoms, or assisted reproductive technologies (ART) to help achieve pregnancy.
Women who are concerned about their fertility and have been diagnosed with subserosal fibroids should speak with their healthcare provider to discuss the best course of treatment for their specific situation.
Conclusion
Subserosal fibroids are benign tumors that grow on the outside of the uterus. They can cause various symptoms and complications depending on their size, number, and location. Subserosal fibroids can be diagnosed by different imaging tests and treated by different methods depending on your individual situation and preferences. Some natural or alternative treatments may also help reduce the risk or symptoms of subserosal fibroids, but they should be used with caution and under medical supervision.
If you have subserosal fibroids or suspect that you may have them, you should consult your doctor for a proper diagnosis and treatment plan. Subserosal fibroids are not life-threatening in most cases, but they can affect your quality of life and health if left untreated. With proper care and management, you can live a healthy and happy life with subserosal fibroids.
FAQs
Q: What is a subserosal fibroid?
A: A subserosal fibroid is a type of uterine fibroid that grows on the outer surface of the uterus, towards the abdominal cavity.
Q: Is subserosal fibroid dangerous?
A: In most cases, subserosal fibroids are not dangerous and do not require treatment. However, if they grow very large or cause symptoms such as pain or heavy bleeding, treatment may be necessary.
Q: Can I get pregnant with subserosal fibroid?
A: Yes, most women with subserosal fibroids are able to conceive and carry a pregnancy to term. However, subserosal fibroids can sometimes impact fertility depending on their size, location, and number.
Q: Can subserosal fibroid cause infertility?
A: Subserosal fibroids can sometimes impact fertility depending on their size, location, and number. If a subserosal fibroid is located near the fallopian tubes, it may cause blockages or prevent the egg from being released properly.
Q: Can subserosal fibroid cause miscarriage?
A: Subserosal fibroids are not typically associated with an increased risk of miscarriage, but larger subserosal fibroids may increase the risk of preterm labor or delivery.
Q: Can subserosal fibroid prevent pregnancy?
A: In most cases, subserosal fibroids do not prevent pregnancy. However, if they grow very large or cause symptoms such as pain or heavy bleeding, treatment may be necessary to improve fertility.
Q: What causes subserosal fibroid?
A: The exact cause of subserosal fibroids is unknown, but they are thought to develop due to genetic factors and hormonal imbalances.
Q: What is an anterior subserosal fibroid?
A: An anterior subserosal fibroid is a type of subserosal fibroid that grows on the front of the uterus, towards the abdominal cavity
Latest Posts
- NVS Staff Nurse Vacancy 2024 – How to Apply

- AIIMS NORCET 6 and ESIC Nursing Exam Questions and Answers


- ESIC Nursing Officer Recruitment 2024 | 1930 Vacancies – Apply Now



- Dream Job Alert: AIIMS NORCET Nursing Officer Vacancy 2024 – Apply Now!



- NIMHANS Nursing Officer Exam 17-12-2023 Memory-Based Solved Questions