Chronic obstructive pulmonary disease (COPD) is a chronic lung disease that can have a significant impact on a patient’s quality of life. COPD is a progressive disease that causes airflow obstruction in the lungs, making it difficult for patients to breathe. Nursing care is critical in the management and treatment of COPD patients.
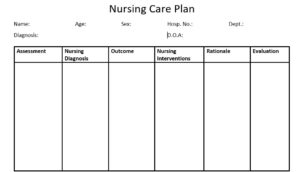
A comprehensive nursing care plan that addresses the patient’s physical, emotional, and psychological needs is essential to improve their overall health and well-being. This article will outline the key components of a nursing care plan for COPD patients, including assessment, diagnosis, nursing interventions, evaluation, and monitoring, as well as the importance of family involvement and collaborative care.
Table of Contents
Understanding COPD: Causes, Symptoms, and Diagnosis
Definition of COPD
COPD, or Chronic Obstructive Pulmonary Disease, is a progressive lung disease that makes it difficult to breathe. It is characterized by chronic bronchitis and emphysema, which causes damage to the air sacs and airways in the lungs.
Types of COPD
COPD is a broad term that encompasses several different lung conditions. The two primary types of COPD are chronic bronchitis and emphysema. Chronic bronchitis is characterized by a persistent cough and excess mucus production, while emphysema is characterized by damage to the air sacs in the lungs, which can cause shortness of breath.
Classification of Severity of Obstructions
The severity of COPD is classified based on the patient’s lung function, as determined by spirometry testing. If a person with COPD has a ratio of FEV1 (forced expiratory volume in one second) to FVC (forced vital capacity) that is less than 0.7, it means they have some degree of airflow limitation. To determine how severe the limitation is, doctors will use the post-bronchodilator value of FEV1.
The severity of the airflow obstruction is then classified using a grading system called GOLD. This system helps doctors understand how serious the person’s COPD is and what treatments may be necessary.
- GOLD 1: Mild (FEV1 greater than 80% of what is predicted for the person’s age and size)
- GOLD 2: Moderate (FEV1 between 50% and 80% of predicted)
- GOLD 3: Severe (FEV1 between 30% and 50% of predicted)
- GOLD 4: Very severe (FEV1 less than 30% of predicted)
The GOLD system helps doctors determine how serious a person’s COPD is and what treatments may be necessary to manage it.
Main Causes of COPD
The main causes of COPD are cigarette smoking, exposure to air pollution, and long-term exposure to chemicals and dust in the workplace. Genetics can also play a role in the development of COPD.
Common Symptoms of COPD
The common symptoms of COPD include shortness of breath, coughing, wheezing, and chest tightness. COPD can also cause fatigue, weight loss, and difficulty sleeping.
Diagnosis of COPD
COPD is diagnosed through a series of tests including spirometry, chest X-rays, and CT scans. These tests help to assess lung function and identify any damage or inflammation in the lungs.
Importance of Nursing Care Plan in COPD Management
Goals of Nursing Care Plan in COPD
The goals of a nursing care plan for COPD patients include improving lung function, managing symptoms, and preventing complications. The nursing care plan also aims to enhance the patient’s physical and emotional well-being, improve their quality of life, and promote self-management of the disease.
Benefits of Nursing Management in COPD
Nursing management in COPD can help patients better understand their disease, manage their symptoms effectively, and reduce their risk of complications. It can also improve their physical and psychological outcomes and enhance their overall quality of life.
Planning for COPD Nursing Care: Assessment and Diagnosis
Physical Assessment of COPD Patients
Physical assessment of COPD patients includes lung function tests, respiratory rate, oxygen saturation, and chest auscultation. The assessment also includes an evaluation of the patient’s nutritional status, exercise tolerance, and overall functional capacity.
Psychological Assessment of COPD Patients
Psychological assessment of COPD patients includes an evaluation of their mental health, cognitive function, and emotional well-being. It helps to identify any psychological or social factors that may affect the patient’s ability to manage their disease and cope with the challenges of living with COPD.
Diagnosis and Care Planning for COPD Patients
The diagnosis and care planning for COPD patients involve the development of a personalized care plan based on the patient’s individual needs and preferences. The care plan includes a range of interventions to manage symptoms, prevent complications, and improve the patient’s overall quality of life.
Nursing Diagnoses
When creating a nursing care plan for COPD, it is essential to consider the patient’s nursing diagnosis. Some common nursing diagnoses for COPD patients include:
- Ineffective Airway Clearances: related to increased production of mucus and coughing as evidenced by wheezing and difficulty breathing.
- Impaired Gas Exchange: related to damage to the alveoli and decreased lung function as evidenced by low oxygen saturation levels and shortness of breath.
- Ineffective Breathing Pattern: related to increased airway resistance and fatigue as evidenced by rapid breathing and use of accessory muscles.
- Imbalanced Nutrition, Less than Body Requirements: related to difficulty breathing and decreased appetite as evidenced by weight loss and poor dietary intake.
- Risk for Infection: related to the weakened immune system and frequent respiratory infections as evidenced by fever and elevated white blood cell count.
- Knowledge Deficit: related to a lack of understanding of COPD and its management as evidenced by patient questions and concerns.
- Activity Intolerance: related to decreased lung function and shortness of breath as evidenced by fatigue and limited physical activity.
- Self-Care Deficit: related to a limited ability to perform activities of daily living as evidenced by difficulty with grooming and dressing.
- Ineffective Coping: related to chronic illness and changes in lifestyle as evidenced by depression and anxiety.
1. Ineffective Airway Clearances:
- May be related to: Increased production of mucus and coughing.
- Possibly evidenced by: Wheezing and difficulty breathing.
- Desired outcomes: The patient will be able to clear their airway effectively.
- Assessment: Monitor the patient’s breathing, coughing, and mucus production. Auscultate lung sounds.
- Nursing interventions:
- Encourage the patient to cough and deep breathe to help clear their airway.
- Administer bronchodilators as ordered to open airways.
- Assist with chest physiotherapy and postural drainage as needed to help loosen and remove mucus.
- Encourage the patient to increase fluid intake to help thin mucus.
- Monitor the patient for signs of respiratory distress and provide supplemental oxygen as needed.
- Rationale: These interventions help to clear mucus and promote effective breathing.
2. Impaired Gas Exchange:
- May be related to: Damage to the alveoli and decreased lung function.
- Possibly evidenced by: Low oxygen saturation levels and shortness of breath.
- Desired outcomes: The patient will maintain adequate oxygen levels and improve respiratory status.
- Assessment: Monitor oxygen saturation levels, respiratory rate, and breath sounds. Assess for signs of cyanosis.
- Nursing interventions:
- Administer supplemental oxygen as ordered to improve oxygenation.
- Encourage the patient to breathe deeply and cough to help clear airways.
- Monitor the patient’s response to medication therapy and report any adverse reactions.
- Provide education on breathing techniques to promote effective gas exchange.
- Monitor and maintain proper positioning to optimize breathing and gas exchange.
- Rationale: These interventions promote effective gas exchange and improve respiratory status.
3. Ineffective Breathing Pattern:
- May be related to: Increased airway resistance and fatigue.
- Possibly evidenced by: Rapid breathing and use of accessory muscles.
- Desired outcomes: The patient will exhibit a regular and normal breathing pattern.
- Assessment: Monitor respiratory rate and depth, use of accessory muscles, and chest expansion.
- Nursing interventions:
- Encourage the patient to take slow, deep breaths and provide relaxation techniques to promote normal breathing patterns.
- Administer bronchodilators and other respiratory medications as ordered to relieve airway resistance.
- Monitor oxygen saturation levels and provide supplemental oxygen as needed.
- Position the patient comfortably to optimize breathing.
- Rationale: These interventions help to promote normal breathing patterns and relieve airway resistance.
4. Imbalanced Nutrition, Less than Body Requirements:
- May be related to: Difficulty breathing and decreased appetite.
- Possibly evidenced by: Weight loss and poor dietary intake.
- Desired outcomes: The patient will achieve and maintain adequate nutrition and hydration.
- Assessment: Monitor the patient’s weight, dietary intake, and fluid intake.
- Nursing interventions:
- Provide small, frequent meals that are high in calories and protein.
- Encourage the patient to eat slowly and rest before and after meals.
- Provide oral care before meals to stimulate appetite.
- Assess the patient’s ability to swallow and provide a modified diet as needed.
- Monitor fluid intake and encourage the patient to drink fluids between meals.
- Rationale: These interventions promote adequate nutrition and hydration.
5. Risk for Infection:
- May be related to: Weakened immune system and frequent respiratory infections.
- Possibly evidenced by: Fever and elevated white blood cell count.
- Desired outcomes: The patient will remain free from respiratory infections.
- Assessment: Monitor the patient’s temperature, white blood cell count, and respiratory status.
- Nursing interventions:
- Monitor the patient for signs of infection and report any changes to the healthcare
- provider. – Ensure proper hand hygiene is practiced by all staff and visitors. – Provide education to the patient and family on infection prevention techniques. – Encourage the patient to get necessary vaccinations, such as the flu vaccine. – Administer antibiotics and antivirals as ordered to prevent or treat infections.
- Rationale: These interventions help to prevent respiratory infections and promote overall health.
6. Knowledge Deficit:
- May be related to: Lack of understanding of COPD and its management.
- Possibly evidenced by: Inability to explain COPD or its treatment plan.
- Desired outcomes: The patient will understand COPD and its management plan.
- Assessment: Assess the patient’s knowledge and understanding of COPD and its management plan.
- Nursing interventions:
- Provide education on COPD and its management plan, including medication regimens and breathing techniques.
- Provide written materials to reinforce education.
- Encourage the patient to ask questions and seek clarification.
- Provide referrals to community resources and support groups.
- Rationale: These interventions help to increase the patient’s knowledge and understanding of COPD and its management plan.
7. Activity Intolerance:
- May be related to: Shortness of breath and decreased lung function.
- Possibly evidenced by: Fatigue and decreased endurance.
- Desired outcomes: The patient will be able to tolerate activities of daily living.
- Assessment: Assess the patient’s level of activity and tolerance.
- Nursing interventions:
- Encourage the patient to engage in light exercise and physical activity, such as walking or stretching.
- Monitor oxygen saturation levels before, during, and after activity.
- Gradually increase activity levels as tolerated.
- Provide education on energy conservation techniques.
- Refer to physical therapy as needed.
- Rationale: These interventions help to improve the patient’s physical conditioning and tolerance for activity.
8. Self-Care Deficit:
- May be related to: Decreased physical ability and fatigue.
- Possibly evidenced by: Difficulty performing activities of daily living independently.
- Desired outcomes: The patient will be able to perform activities of daily living independently.
- Assessment: Assess the patient’s ability to perform self-care activities, such as grooming and dressing.
- Nursing interventions:
- Provide education on energy conservation techniques and assistive devices to promote independence.
- Encourage the patient to practice self-care activities as much as possible.
- Provide referrals to occupational therapy as needed.
- Assess the need for home health services.
- Rationale: These interventions help to promote independence and improve the patient’s ability to perform self-care activities.
9. Ineffective Coping:
- May be related to: Fear and anxiety related to COPD diagnosis.
- Possibly evidenced by: Reports of increased stress and difficulty managing COPD.
- Desired outcomes: The patient will effectively cope with the diagnosis of COPD.
- Assessment: Assess the patient’s coping mechanisms and stress levels.
- Nursing interventions:
- Provide education on stress management techniques and coping strategies.
- Encourage the patient to seek support from family, friends, and support groups.
- Provide referrals to counseling services as needed.
- Monitor the patient’s emotional well-being and provide support.
- Rationale: These interventions help to improve the patient’s ability to cope with the diagnosis of COPD and promote emotional well-being.
10. Risk for Falls:
- May be related to: Fatigue, shortness of breath, and decreased mobility.
- Possibly evidenced by: History of falls or near falls, and unsteady gait.
- Desired outcomes: The patient will remain free from falls.
- Assessment: Assess the patient’s risk for falls, including mobility and balance.
- Nursing interventions:
- Implement fall prevention measures, such as bed alarms and non-slip socks.
- Assist with mobility as needed.
- Provide education on fall prevention techniques, such as using assistive devices and wearing appropriate footwear.
- Refer to physical therapy as needed.
- Rationale: These interventions help to prevent falls and promote patient safety.
11. Impaired Skin Integrity:
- May be related to: Immobility and decreased oxygenation to tissues.
- Possibly evidenced by: Skin breakdown, and pressure ulcers.
- Desired outcomes: The patient will maintain intact skin.
- Assessment: Assess the patient’s skin integrity and risk for pressure ulcers.
- Nursing interventions:
- Turn and reposition the patient every 2 hours or as needed.
- Use pressure-reducing devices, such as foam wedges or cushions.
- Assess and treat any areas of skin breakdown.
- Provide education on skincare and pressure ulcer prevention.
- Rationale: These interventions help to maintain skin integrity and prevent pressure ulcers.
12. Impaired Social Interaction:
- May be related to: Decreased mobility and social isolation.
- Possibly evidenced by: Lack of social support or participation in activities.
- Desired outcomes: The patient will participate in social activities and maintain social connections.
- Assessment: Assess the patient’s social support and participation in activities.
- Nursing interventions:
- Encourage participation in social activities, such as games or crafts.
- Facilitate communication with family and friends.
- Provide referrals to support groups and community resources.
- Rationale: These interventions help to improve the patient’s social interactions and prevent social isolation.
In conclusion, the nursing care plan for COPD includes various nursing diagnoses, including ineffective airway clearance, impaired gas exchange, ineffective breathing pattern, imbalanced nutrition, less than body requirements, the risk for infection, knowledge deficit, activity intolerance, self-care deficit, ineffective coping, the risk for falls, impaired skin integrity, and impaired social interaction.
To address these nursing diagnoses, nursing interventions such as providing education, administering medications, implementing fall prevention measures, and encouraging physical activity and social interaction may be utilized. Regular assessment and evaluation of the patient’s condition are also crucial for the success of the nursing care plan.
FAQs
Q: What is a nursing care plan for COPD?
A: A nursing care plan for COPD is a written document that outlines the nursing interventions and actions needed to manage a patient’s symptoms and improve their quality of life. The plan includes specific goals, interventions, and expected outcomes based on the patient’s individual needs.
Q: What are some common nursing diagnoses for COPD patients?
A: Common nursing diagnoses for COPD patients include ineffective airway clearance, impaired gas exchange, ineffective breathing pattern, imbalanced nutrition, the risk for infection, knowledge deficit, activity intolerance, self-care deficit, and ineffective coping.
Q: What are some nursing interventions for COPD patients with ineffective airway clearance?
A: Nursing interventions for COPD patients with ineffective airway clearance may include encouraging deep breathing and coughing, providing chest physiotherapy, administering bronchodilators, and suctioning secretions as needed.
Q: What are some nursing interventions for COPD patients with impaired gas exchange?
A: Nursing interventions for COPD patients with the impaired gas exchange may include positioning the patient for optimal breathing, administering oxygen therapy as prescribed, monitoring oxygen saturation levels, and encouraging regular exercise.
Q: What are some nursing interventions for COPD patients with imbalanced nutrition?
A: Nursing interventions for COPD patients with imbalanced nutrition may include providing small, frequent meals, monitoring fluid intake, encouraging high-calorie, high-protein foods, and collaborating with a registered dietitian for nutritional support.
Q: What are some nursing interventions for COPD patients with a risk for infection?
A: Nursing interventions for COPD patients with a risk for infection may include teaching the patient and family members proper hand hygiene, encouraging regular vaccination, administering antibiotics as prescribed, and monitoring for signs of infection.
Q: How can a nursing care plan help manage COPD symptoms?
A: A nursing care plan can help manage COPD symptoms by providing a structured approach to care that focuses on the patient’s individual needs. The plan includes specific goals and interventions designed to improve the patient’s breathing, reduce the risk of complications, and enhance their quality of life.
Q: Who develops a nursing care plan for COPD patients?
A: A nursing care plan for COPD patients is typically developed by a registered nurse in collaboration with other healthcare professionals, including physicians, respiratory therapists, and dietitians. The plan is based on a comprehensive assessment of the patient’s physical, emotional, and social needs.
- NVS Staff Nurse Vacancy 2024 – How to Apply
- AIIMS NORCET 6 and ESIC Nursing Exam Questions and Answers
- ESIC Nursing Officer Recruitment 2024 | 1930 Vacancies – Apply Now
- Dream Job Alert: AIIMS NORCET Nursing Officer Vacancy 2024 – Apply Now!
- NIMHANS Nursing Officer Exam 17-12-2023 Memory-Based Solved Questions